Estrogen
 From Nwe
From Nwe Estrogens (also oestrogens) are a group of steroid (type of lipid) compounds that function as the primary female sex hormone. Estrogens are named for their importance in the estrous cycle. The estrous cycle (also oestrous cycle) refers to the recurring physiologic changes that are induced by reproductive hormones in most mammalian placental females; humans and some primates, bats, and shrews are the only mammals who undergo a menstrual cycle instead. Estrogens are important in both those mammals undergoing an estrous cycle and those undergoing a menstrual cycle.
In humans, while estrogens are present in both men and women, they are usually present at significantly higher levels in women of reproductive age. They promote the development of female secondary sex characteristics, such as breasts, and are also involved in the thickening of the endometrium and other aspects of regulating the menstrual cycle. Follicle stimulating hormone (FSH) and luteinizing hormone (LH) regulate the production of estrogen in ovulating women. Since estrogen circulating in the blood can feedback to reduce circulating levels of FSH and LH, some oral contraceptives contain estrogens to prevent ovulation.
Part of the endocrine system, estrogen production and function reveals the complexity and harmony of the body. Produced in one part of the body, estrogen travels to other parts and binds to specific receptors in order to function. There is concern that some synthetic environmental chemicals, such as found in agricultural and home chemicals (insecticides, herbicides, fungicides, etc.) and industrial chemicals (detergents, resins) may interfere with this complex coordination and hormonal messenger system. There is likewise concern about unintended consequences of synthetic estrogens used to mimic estrogen. For example, between 1938 and 1971 in the United States, a synthetic estrogen, diethylstilbestrol, was prescribed to women to prevent miscarriages, but was later correlated with the development of cancers in the offspring and the women themselves (Schrager and Potter 2004).
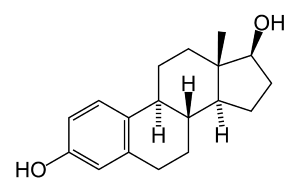
The three major naturally occurring estrogens in women are estradiol, estriol, and estrone. From menarche (woman's first menstrual period) to menopause (the cessation of menstrual periods), the primary estrogen is estradiol 17beta. In the body, these types of estrogens are mainly produced from androgens, which are produced in the adrenal glands, and then converted to estrogen componds through enzyme action. Estradiol is produced from testosterone and estrone from androstenedione. Estrone is weaker than estradiol, and in post-menopausal women, more estrone is present than estradiol.
Estrogen Production
In human females, estrogen is produced primarily by developing follicles in the ovaries, the corpus luteum, and the placenta during pregnancy. Some estrogens are also produced in smaller amounts by other tissues such as the liver, adrenal glands, and the breasts. These secondary sources of estrogen are especially important in post-menopausal women. Synthesis of oestrogenes starts in theca interna cells in the ovary, by the synthesis of androstenedione from cholesterol. Androstenedione is a substance of moderate androgenic activity. This compound crosses the basal membrane into the surrounding granulosa cells, where it is converted to estrone or estradiol, either immediately or through testosterone.
Dehydroepiandrosterone (DHEA) is an abundant sex steroid in women and like other steroids is efficiently sulfated. DHEA is a precursor steroid that can be converted to estrogens (estradiol) and androgens, such as testosterone and dihydrotestosterone (5α-dihydrotestosterone), and it has been known to have a large effect on increasing female sexual desire. Estrogens can also be produced by the enzyme aromatase, which converts androgens such as DHEA to estrogens, mainly estradiol and estrone.
In human males, estrogen is produce in the testicles and is found in the sperm. Too much estrogen in males can inhibit the growth of the testes and production of sperm (Douglas et al. 1996).
Functions of Estrogen
Estrogen serves several purposes and has many different functions, which are touched upon below.
- Structural
There are four main structural functions of estrogen. First, it stimulates endometrial growth during the menstrual cycle. Second, it is responsible for the maintenance of blood vessels and the skin. Third, estrogen reduces bone resorption, therefore increasing bone formation. This function of estrogen affects post-menopausal women greatly since a lack of estrogen is associated with osteoporosis (a disease of the bone). Last, estrogen increases uterine growth.
- Protein synthesis
Estrogen helps to increase hepatic (liver) production of binding proteins.
- Coagulation
Coagulation, when referring to blood, is its ability to form a clot(s). Estrogen increases the circulating level of factors 2, 7, 9, 10, anti-thrombin III, and plasminogen. These chemical factors play a role in the coagulation cascade and are necessary for blood clotting. Estrogen also increases platelet adhesiveness.
- Lipid
Estrogen increases HDL (also known as good cholesterol), lipids (triglycerides), and fat deposits. It decreases LDL (bad cholesterol) levels.
- Fluid balance
Salt and water retention are caused by estrogen.
- Gastrointestinal (GI)
Reduced bowel motility and increased levels of cholesterol in bile are consequences of estrogen.
Medical Applications
A range of synthetic and natural substances have been identified that possess estrogenic activity. These include bisphenol-A, phthalate esters, and nonylphenol.
Estrogen replacement therapy has proven to be a very useful method of treating osteoporosis in postmenopausal women, as well as the symptoms of menopause, such as hot flushes, vaginal dryness, urinary stress incontinence, chilly sensations, dizziness, fatigue, irritability, and sweating. Fractures of the spine, wrist, and hips decrease by 50-70 percent and spinal bone density increases by around five percent in those women treated with estrogen within three years of the onset of menopause and for 5-10 years thereafter. Standard therapy is 0.625 mg/day of conjugated estrogens (such as is in Premarin), but the dose can range from 0.3 mg/day to 1.25 mg/day. Estrogen replacement therapy also has favorable effects on serum cholesterol levels and is claimed to dramatically reduce the incidence of cardiovascular disease.
There are, however, risks associated with estrogen therapy. Among the older postmenopausal women studied as part of the Women's Health Initiative (WHI), an orally-administered estrogen supplement has been associated with an increased risk of dangerous blood clotting. The WHI studies used one type of estrogen supplement, a high oral dose of conjugated equine estrogens (Premarin alone and with Provera as Prempro)[1] It is yet to be determined if risks of estrogen supplement use are the same for all estrogen supplement types. In particular, topically-applied estrogen may have a different spectrum of side-effects than does estrogen administered by the oral route (Menon and Vongpatanasin 2006).
Another very popular medical application of estrogen is the combined administration of it with progestins in the application of oral contraceptives.
Other uses include therapy involving vaginal atrophy, hypoestrogenism (as a result of hypogonadism, castration, or primary ovarian failure), amenorrhea, dysmenorrhea, and oligomenorrhea. Estrogens can also be used to suppress lactation after child birth.
Boxed warning
The labeling of estrogen-only products in the United States includes a black box warning that unopposed estrogen (without progestin) therapy increases the risk of endometrial cancer.
Based on a review of data from the WHI, on January 8, 2003 the Food and Drug Administration of the United States changed the labeling of all estrogen and estrogen with progestin products for use by postmenopausal women to include a new boxed warning about cardiovascular and other risks. The estrogen-alone substudy of the WHI reported an increased risk of stroke and deep vein thrombosis (DVT) in postmenopausal women 50 years of age or older and an increased risk of dementia in postmenopausal women 65–years–of–age or older using 0.625 mg of Premarin conjugated equine estrogens (CEE). The estrogen-plus-progestin substudy of the WHI reported an increased risk of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and DVT in postmenopausal women 50–years–of–age or older and an increased risk of dementia in postmenopausal women 65–years–of–age or older using 0.625 mg of CEE with 2.5 mg of the progestin medroxyprogesterone acetate (MPA) (FDA 2003, MedlinePlus 2003, Kolata 2003).
Notes
- ↑ Menopausal Hormone Therapy Information, Department of Health and Human Services, 2008, Retrieved January 21, 2008
References
ISBN links support NWE through referral fees
- Braunstein, G. D., et al. Safety and efficacy of a testosterone patch for the treatment of hypoactive sexual desire disorder in surgically menopausal women: a randomized, placebo-controlled trial. Archives of Internal Medicine 165(14) (2005):1582-9. PMID 16043675.
- Davis, S. R., S. Donath, and R. J. Bell. "Circulating androgen levels and self-reported sexual function in women" Journal of the American Medical Association 294(1) (2005):91-6.
- Douglas, C., M. Moore, and Rosalind Schoof. "Endocrine disruptors and other scary things" The Seattle Daily Journal of Commerce. August 22, 1996.
- Fang, H., W. Tong, et al. "Structure-activity relationships for a large diverse set of natural, synthetic, and environmental estrogens" Chemical Research in Toxicology 14 (2001):280-294. PMID 11258977.
- Kolata, G. "F.D.A. orders warning on all estrogen labels" The New York Times. January 9, 2003.
- Massaro, D., and G. D. Massaro. "Estrogen regulates pulmonary alveolar formation, loss, and regeneration in mice" American Journal of Physiology. Lung Cellular and Molecular Physiology 287(6) (2004):L1154-9. PMID 15298854.
- MedlinePlus. Important Warning. U.S. National Library of Medicine and National Institutes of Health, 2006. Retrieved March 19, 2022.
- Menon, D. V., and W. Vongpatanasin. "Effects of transdermal estrogen replacement therapy on cardiovascular risk factors" Treat Endocrinol. 5(1) (2006):37-51.
- Schrager, S., and B. E. Potter. Diethylstilbestrol exposure. American Family Physician 69(10)(2004):2395-2404.
- Warnock, J. K., et al. "Combined esterified estrogens and methyltestosterone versus esterified estrogens alone in the treatment of loss of sexual interest in surgically menopausal women" Menopause. 12(4) (2005):374-84. PMID 16037752.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
↧ Download as ZWI file | Last modified: 02/04/2023 05:32:27 | 44 views
☰ Source: https://www.newworldencyclopedia.org/entry/Estrogen | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed: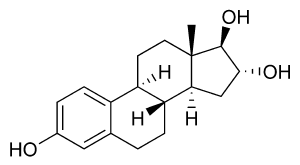
 KSF
KSF