Periorbital Cellulitis
 From Mdwiki
From Mdwiki | Periorbital cellulitis | |
|---|---|
| Other names: Preseptal cellulitis | |
.JPG) | |
| Periorbital cellulitis around the left eye | |
| Symptoms | Tender, red, and swollen eyelid[1] |
| Complications | Rare, orbital cellulitis[2] |
| Usual onset | Sudden[3] |
| Causes | Breaks in the skin around the eye, sinusitis[1][4] |
| Diagnostic method | Based on symptoms, medical imaging in unclear cases[4] |
| Differential diagnosis | Orbital cellulitis, hay fever, chalazion, hordeolum[4][2] |
| Treatment | Antibiotics, such as amoxicillin/clavulanate[5] |
| Frequency | Relatively common[4] |
Periorbital cellulitis, also known as preseptal cellulitis, is an infection of the eyelid and tissue anterior to the orbital septum.[4] Symptoms may include a tender, red, and swollen eyelid.[1] Fever is less commonly present.[4] Vision should be normal and movement of the eye should occur without difficulty.[1] Complications are rare, though occasionally include orbital cellulitis.[2]
It typically occurs following a breaks in the skin around the eye, such as from scratching or an insect bite.[1] It may also occur as a complication of a chalazion or sinusitis.[4] Diagnosis is based on symptoms, with medical imaging done in unclear cases.[4]
Those with mild disease may be treated with antibiotics by mouth such as amoxicillin/clavulanate for 7 to 10 days.[3][5] Clindamycin or trimethoprim/sulfamethoxazole may be added if MRSA is a concern.[4] With treatment, it should resolve within a week.[2]
Periorbital cellulitis is relatively common in comparison to orbital cellulitis.[4] Children are more commonly affected than adults.[2] In children it represents about 85% of swelling around the eye.[3] While the term could mean any swelling around the eye, it is technically only used for cases related to infection.[3]
Signs and symptoms[edit | edit source]
Symptoms may include swelling, redness, discharge, pain, conjunctival infection, and occasionally fever.
Typical signs include periorbital erythema, induration, tenderness and warmth.[6]
Causes[edit | edit source]
Staphylococcus aureus, Streptococcus pneumoniae, other streptococci, and anaerobes are the most common causes, depending on the origin of the infection.[7]
Diagnosis[edit | edit source]
If the diagnosis is unclear, a CT scan may be done to rule out other possibilities.
Periorbital cellulitis caused by a dental infection (also causing maxillary sinusitis)
Differential diagnosis[edit | edit source]
Periorbital cellulitis must be differentiated from orbital cellulitis. In contrast to orbital cellulitis, periorbital cellulitis do not have bulging of the eye (proptosis), limited eye movement (ophthalmoplegia), pain on eye movement, or loss of vision.
Prevention[edit | edit source]
The use of the Haemophilus influenzae vaccine has decreased the rate.[8]
Treatment[edit | edit source]
Antibiotics are aimed at gram positive bacteria. Medical attention should be sought if symptoms persist beyond 2–3 days.
There is inadequate evidence regarding adding corticosteroids in the treatment of periorbital cellulitis as of 2021.[9]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Baiu, Ioana; Melendez, Elliot (14 January 2020). "Periorbital and Orbital Cellulitis". JAMA. 323 (2): 196. doi:10.1001/jama.2019.18211.
- ↑ 2.0 2.1 2.2 2.3 2.4 Bae, C; Bourget, D (January 2023). "Periorbital Cellulitis". StatPearls. PMID 29261970.
- ↑ 3.0 3.1 3.2 3.3 Williams, Katherine J.; Allen, Richard C. (September 2019). "Paediatric orbital and periorbital infections". Current Opinion in Ophthalmology. 30 (5): 349–355. doi:10.1097/ICU.0000000000000589.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 "Preseptal and Orbital Cellulitis - Eye Disorders". Merck Manuals Professional Edition. Archived from the original on 1 December 2022. Retrieved 2 July 2023.
- ↑ 5.0 5.1 Gordon, Abigail A.; Phelps, Paul O. (October 2020). "Management of preseptal and orbital cellulitis for the primary care physician". Disease-a-Month. 66 (10): 101044. doi:10.1016/j.disamonth.2020.101044. PMID 32622679.
- ↑ Givner LB (December 2002). "Periorbital versus orbital cellulitis". The Pediatric Infectious Disease Journal. 21 (12): 1157–1158. doi:10.1097/00006454-200212000-00014. PMID 12488668.
- ↑ Botting AM, McIntosh D, Mahadevan M (March 2008). "Paediatric pre- and post-septal peri-orbital infections are different diseases. A retrospective review of 262 cases". International Journal of Pediatric Otorhinolaryngology. 72 (3): 377–383. doi:10.1016/j.ijporl.2007.11.013. PMID 18191234.
- ↑ Donahue SP, Schwartz G (October 1998). "Preseptal and orbital cellulitis in childhood. A changing microbiologic spectrum". Ophthalmology. 105 (10): 1902–5, discussion 1905–6. doi:10.1016/S0161-6420(98)91038-7. PMID 9787362.
- ↑ Kornelsen E, Mahant S, Parkin P, Ren LY, Reginald YA, Shah SS, Gill PJ, et al. (Cochrane Eyes and Vision Group) (April 2021). "Corticosteroids for periorbital and orbital cellulitis". The Cochrane Database of Systematic Reviews. 2021 (4): CD013535. doi:10.1002/14651858.CD013535.pub2. PMC 8092453. PMID 33908631.
External links[edit | edit source]
| Classification | |
|---|---|
| External resources |
Categories: [Bacterial diseases] [Periorbital conditions] [RTT]
↧ Download as ZWI file | Last modified: 09/30/2023 14:44:20 | 1 views
☰ Source: https://mdwiki.org/wiki/Periorbital_cellulitis | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed: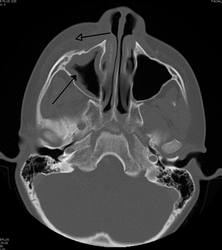
.png)
 KSF
KSF