Chronic Neutrophilic Leukemia
 From Mdwiki
From Mdwiki | Chronic neutrophilic leukemia | |
|---|---|
| Other names: CNL[1] | |
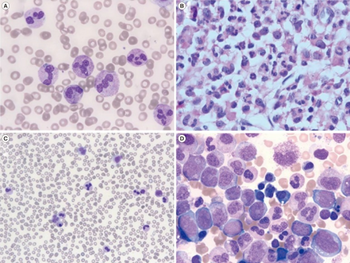 | |
| Chronic neutrophilic leukemia-a) peripheral blood shows neutrophilia b) bone marrow biopsy showing a markedly elevated myeloid:erythroid ratio c) peripheral blood with monocytosis and neutrophilia d) bone marrow aspirate with erythroid and granulocytic dysplasia | |
| Specialty | Hematology and oncology |
Chronic neutrophilic leukemia (CNL) is a rare myeloproliferative neoplasm that features a persistent neutrophilia in peripheral blood, myeloid hyperplasia in bone marrow, hepatosplenomegaly, and the absence of the Philadelphia chromosome or a BCR/ABL fusion gene.[2]
Signs and symptoms[edit | edit source]
The most common clinical finding is hepatosplenomegaly. Pruritus, gout, and mucocutaneous bleeding are occasionally seen.[3][4]
Cause[edit | edit source]
The cause of CNL is currently unknown. An association between CNL and multiple myeloma has been suggested based on the observation of myeloma in 20% of CNL cases.[5] However, a clonal genetic abnormality has not been detected in these myeloma-associated cases of CNL, raising the possibility that the neutrophilia is a reaction due to the neoplastic myeloma cells.[2] The postulated cell of origin is a limited-potential, marrow-derived stem cell.[6]
Genetics[edit | edit source]
The majority (90%) of cases have not had detectable cytogenetic abnormalities. Most importantly, the Philadelphia chromosome and other BCR/ABL fusion genes are not detected.[2]
Diagnosis[edit | edit source]
Laboratory findings[edit | edit source]
Peripheral blood neutrophilia (> 25 x 109/L) with myeloid precursors (promyelocytes, myelocytes, metamyelocytes) comprising less than 5% of leukocytes.[3][4]
Sites of involvement[edit | edit source]
Peripheral blood, bone marrow, spleen, and liver are most common, but any organ or tissue can be infiltrated by neutrophils.[3] [4]
Bone marrow biopsy[edit | edit source]
On both the bone marrow aspirate and the core biopsy, a hypercellular marrow with an increased myeloid:erythroid ratio of 20:1 or greater. Myelocytes and neutrophils are increased, and blasts and promyelocytes are not increased. Due to the myeloproliferative nature of the disease, an increase in megakaryocytes and erythroid precursors may be observed, but dyspoiesis in not seen in any cell lineage. Also, reticulin fibrosis is rare.[3][4] There is a reported association between CNL and multiple myeloma, so the bone marrow biopsy may show evidence of a plasma cell dyscrasia with increased numbers of atypical plasma cells.[2]
Spleen[edit | edit source]
Splenic infiltrates are typically found only in the red pulp.[3] [4]
Liver[edit | edit source]
Hepatic infiltrates can be found in either the sinusoids, portal triad regions, or both.[3][4]
Immunophenotype[edit | edit source]
No distinct immunophenotype abnormality for CNL has been described.[2] See OHSU 2013 findings of gene CSF3R, mutation p. T6181
Treatment[edit | edit source]
In terms of management we find that the available options include:[7]
- Hydroxyurea
- Interferons
- JAK inhibitors
Epidemiology[edit | edit source]
This is a rare disease, with less than 100 cases reported. Of these cases, an equal male:female ratio was observed,[3] with cases typically seen in older adults.[4]
References[edit | edit source]
- ↑ "Chronic neutrophilic leukemia | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 17 November 2019. Retrieved 17 November 2019.
- ↑ 2.0 2.1 2.2 2.3 2.4 Elaine Sarkin Jaffe, Nancy Lee Harris, World Health Organization, International Agency for Research on Cancer, Harald Stein, J.W. Vardiman (2001). Pathology and genetics of tumours of haematopoietic and lymphoid tissues. World Health Organization Classification of Tumors. Vol. 3. Lyon: IARC Press. ISBN 92-832-2411-6. Archived from the original on 2020-08-04. Retrieved 2022-01-30.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 You W, Weisbrot IM (August 1979). "Chronic neutrophilic leukemia. Report of two cases and review of the literature". Am. J. Clin. Pathol. 72 (2): 233–42. doi:10.1093/ajcp/72.2.233. PMID 289288.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Zittoun R, Réa D, Ngoc LH, Ramond S (February 1994). "Chronic neutrophilic leukemia. A study of four cases". Ann. Hematol. 68 (2): 55–60. doi:10.1007/BF01715131. PMID 8148416.
- ↑ Standen GR, Steers FJ, Jones L (April 1993). "Clonality of chronic neutrophilic leukaemia associated with myeloma: analysis using the X-linked probe M27 beta". J. Clin. Pathol. 46 (4): 297–8. doi:10.1136/jcp.46.4.297. PMC 501206. PMID 8098719.
- ↑ Yanagisawa K, Ohminami H, Sato M, et al. (March 1998). "Neoplastic involvement of granulocytic lineage, not granulocytic-monocytic, monocytic, or erythrocytic lineage, in a patient with chronic neutrophilic leukemia". Am. J. Hematol. 57 (3): 221–4. doi:10.1002/(SICI)1096-8652(199803)57:3<221::AID-AJH7>3.0.CO;2-X. PMID 9495373.
- ↑ Thomopoulos, Thomas P.; Symeonidis, Argiris; Kourakli, Alexandra; Papageorgiou, Sotirios G.; Pappa, Vasiliki (14 April 2022). "Chronic Neutrophilic Leukemia: A Comprehensive Review of Clinical Characteristics, Genetic Landscape and Management". Frontiers in Oncology. 12: 891961. doi:10.3389/fonc.2022.891961. Archived from the original on 27 June 2022. Retrieved 23 June 2022.
External links[edit | edit source]
| Classification | |
|---|---|
| External resources |
Categories: [Chronic myeloid leukemia] [Rare cancers]
↧ Download as ZWI file | Last modified: 01/22/2024 13:27:17 | 7 views
☰ Source: https://mdwiki.org/wiki/Chronic_neutrophilic_leukemia | License: CC BY-SA 3.0
 KSF
KSF