Acral Lentiginous Melanoma
 From Mdwiki
From Mdwiki | Acral lentiginous melanoma | |
|---|---|
 | |
| Specialty | Dermatology |
| Symptoms | Areas of dark pigmentation [1] |
| Complications | Ulceration, spread[2] |
| Causes | Malignant melanocytes[3][4] |
| Risk factors | Dark skin[2] |
| Diagnostic method | Biopsy[5] |
| Treatment | Biologic immunotherapy agents[6] |
| Frequency | Males = females[2] |
Acral lentiginous melanoma is a type of skin cancer.[2] It typically begins as a uniform brownish mark before becoming darker and wider with a blurred irregular edge, most frequently seen in the foot of a person with darker skin.[2] It may become bumpy and ulcerate.[2] Just under the nails and the fingers can also be affected, and it may spread.[2]
It arises from pigment cells (melanocytes).[7] Acral lentiginous melanoma is the most common subtype in people with darker skins and is rare in people with lighter skin types. Acral lentiginous melanoma is observed on the palms, soles, under the nails and in the oral mucosa. It occurs on non-hair-bearing surfaces of the body, which have not necessarily been exposed to sunlight. It is also found on mucous membranes.[8] The average age at diagnosis is between 60 and 70 years.[9]
Acral lentiginous melanoma is the most common form of melanoma diagnosed amongst Asian and sub-Saharan African ethnic groups.[10] 60% occur in the nails, palms and soles.[2] Males and females are affected equally.[2]
Signs and symptoms[edit | edit source]
Typical signs of acral lentiginous melanoma include the following [1]
- Longitudinal tan, black, or brown streak on a nail
- Pigmentation of proximal nail fold
- Areas of dark pigmentation (palms of hands)
Warning signs are new areas of pigmentation, or existing pigmentation that shows change. If caught early, acral lentiginous melanoma has a similar cure rate as the other types of superficial spreading melanoma.[11]
Skin[edit | edit source]
-
Acral lentiginous melanoma
-
Acral lentiginous melanoma
-
Acral lentiginous melanoma
-
-
-
Nails[edit | edit source]
Acral lentiginous melanoma may present as a dark mark under a nail, or a black mark in the nail fold at the end of a dark streak.[2] There may be Hutchinson's sign.[2]
Causes[edit | edit source]
Acral lentiginous melanoma is a result of malignant melanocytes at the membrane of the skin (outer layers).[3][4] The pathogenesis of acral lentiginous melanoma remains unknown at this time.[12]
Diagnosis[edit | edit source]
Although the ideal method of diagnosis of melanoma is complete excisional biopsy,[13] alternatives may be required according to the location of the melanoma. Dermatoscopy of acral pigmented lesions is very difficult but can be accomplished with diligent focus. Initial confirmation of the suspicion can be done with a small wedge biopsy or small punch biopsy.[5] Thin deep wedge biopsies can heal very well on acral skin, and small punch biopsies can give enough clue to the malignant nature of the lesion. Once this confirmatory biopsy is done, a second complete excisional skin biopsy can be performed with a narrow surgical margin (1 mm). This second biopsy will determine the depth and invasiveness of the melanoma,[14] and will help to define what the final treatment will be. If the melanoma involves the nail fold and the nail bed, complete excision of the nail unit might be required. Final treatment might require wider excision (margins of 0.5 cm or more), digital amputation, lymphangiogram with lymph node dissection, or chemotherapy.[15]
Dermoscopy[edit | edit source]
-
-
Acral lentiginous melanoma dermoscopy
-
Parallel ridge pattern with diffuse pigmentation
-
Ridge pattern, asymmetry of structures and colours
-
Parallel ridge pattern
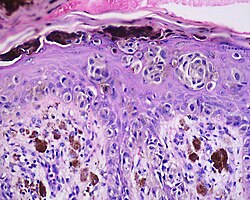
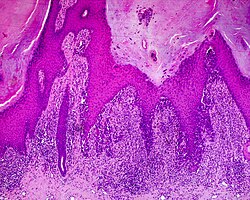
Histology[edit | edit source]
The main characteristic of acral lentiginous melanoma is continuous proliferation of atypical melanocytes at the dermoepidermal junction.[16] Other histological signs of acral lentiginous melanoma include dermal invasion and desmoplasia.[17]
According to Scolyer et al.,[18] ALM "is usually characterized in its earliest recognisable form as single atypical melanocytes scattered along the junctional epidermal layer".
-
-
Acral lentiginous melanoma (ALM)
Treatment[edit | edit source]
Therapies for metastatic melanoma include the biologic immunotherapy agents ipilimumab, pembrolizumab, and nivolumab; BRAF inhibitors, such as vemurafenib and dabrafenib; and a MEK inhibitor trametinib.[6]
Prognosis[edit | edit source]
It has been demonstrated that acral lentiginous melanoma has a poorer prognosis compared to that of cutaneous malignant melanoma (CMM).[19]
Society[edit | edit source]
Jamaican musician Bob Marley died of the condition in 1981, aged 36.[20]
See also[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Goodheart, Herbert P. (2010-10-25). Goodheart's Same-site Differential Diagnosis: A Rapid Method of Diagnosing and Treating Common Skin Disorders. Lippincott Williams & Wilkins. ISBN 9781605477466. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "30. Melanocytic nevi and neoplasms". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. pp. 696–697. ISBN 978-0-323-54753-6.
- ↑ 3.0 3.1 Brown, Kimberly M.; Chao, Celia (2014). Melanoma. Elsevier Health Sciences. ISBN 9780323326834. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ 4.0 4.1 Piliang, Melissa Peck (June 2011). "Acral Lentiginous Melanoma". Clinics in Laboratory Medicine. 31 (2): 281–288. doi:10.1016/j.cll.2011.03.005. PMID 21549241. – via ScienceDirect (Subscription may be required or content may be available in libraries.)</
- ↑ 5.0 5.1 ChB, David E. Elder MB; PhD, Sook Jung Yun MD (2014-11-10). Superficial Melanocytic Pathology. Demos Medical Publishing. ISBN 9781620700235. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ 6.0 6.1 Maverakis E, Cornelius LA, Bowen GM, Phan T, Patel FB, Fitzmaurice S, He Y, Burrall B, Duong C, Kloxin AM, Sultani H, Wilken R, Martinez SR, Patel F (2015). "Metastatic melanoma - a review of current and future treatment options". Acta Derm Venereol. 95 (5): 516–524. doi:10.2340/00015555-2035. PMID 25520039. Archived from the original on 2018-07-19. Retrieved 2018-11-04.
- ↑ Phan, A.; Touzet, S.; Dalle, S.; Ronger‐Savlé, S.; Balme, B.; Thomas, L. (2007). "Acral lentiginous melanoma: histopathological prognostic features of 121 cases". British Journal of Dermatology. 157 (2): 311–318. doi:10.1111/j.1365-2133.2007.08031.x. ISSN 1365-2133. PMID 17596173.
- ↑ LeBoit, Philip E. (2006). Pathology and Genetics of Skin Tumours. IARC. ISBN 9789283224143. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ Swartz, Mark H. (2014-01-07). Textbook of Physical Diagnosis: History and Examination. Elsevier Health Sciences. ISBN 9780323225076. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ Farage, Miranda A. (2010-01-22). Textbook of Aging Skin. Springer Science & Business Media. ISBN 9783540896555. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ Hearing, Vincent J.; Leong, Stanley P. L. (2007-11-05). From Melanocytes to Melanoma: The Progression to Malignancy. Springer Science & Business Media. ISBN 9781592599943. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ ChB, David E. Elder, MB; PhD, Sook Jung Yun, MD (2014-11-10). Superficial Melanocytic Pathology. Demos Medical Publishing. p. 119. ISBN 9781617051869. Archived from the original on 2021-08-27. Retrieved 11 October 2016.
- ↑ Shea, Christopher R.; Reed, Jon A.; Prieto, Victor G. (2014-11-03). Pathology of Challenging Melanocytic Neoplasms: Diagnosis and Management. Springer. ISBN 9781493914449. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ Barnhill, Raymond L.; Piepkorn, Michael; Busam, Klaus J. (2014-02-18). Pathology of Melanocytic Nevi and Melanoma. Springer Science & Business Media. ISBN 9783642383854. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ Clarke, Loren E.; Clarke, Jennie T.; Helm, Klaus F. (2014-03-01). Color Atlas of Differential Diagnosis in Dermatopathology. JP Medical Ltd. ISBN 9789350908457. Archived from the original on 2021-08-31. Retrieved 2020-12-06.
- ↑ Piliang, Melissa Peck (2009). "Acral Lentiginous Melanoma". Surgical Pathology Clinics. 2 (3): 535–541. doi:10.1016/j.path.2009.08.005. ISSN 1875-9181. PMID 26838538.
- ↑ Mooi, Walter; Krausz, Thomas (2007-09-28). Pathology of Melanocytic Disorders 2ed. CRC Press. ISBN 9781444113808. Archived from the original on 2021-08-27. Retrieved 2020-12-06.
- ↑ "FEBS Press". doi:10.1002/(ISSN)1878-0261. Archived from the original on 2021-08-31. Retrieved 2015-05-23.
- ↑ Bradford, Porcia T.; Goldstein, Alisa M.; McMaster, Mary L.; Tucker, Margaret A. (2009). "Acral Lentiginous Melanoma: Incidence and Survival Patterns in the United States, 1986-2005". Archives of Dermatology. 145 (4): 427–434. doi:10.1001/archdermatol.2008.609. ISSN 0003-987X. PMC 2735055. PMID 19380664.
- ↑ "Bob Marley Shouldn't Have Died from Melanoma". Skin Cancer Foundation. 2016-02-06. Archived from the original on 2019-07-27. Retrieved 2016-10-11.
External links[edit | edit source]
| Classification |
|---|
Categories: [Melanoma]
↧ Download as ZWI file | Last modified: 05/07/2024 19:49:31 | 4 views
☰ Source: https://mdwiki.org/wiki/Acral_lentiginous_melanoma | License: CC BY-SA 3.0
.jpg)
.jpg)
.jpg)



.jpg)
.jpg)
.jpg)

.jpg)
.jpg)
.jpg)
.jpg)
 KSF
KSF