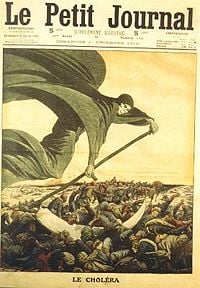
Cholera
 From Nwe
From Nwe |
Vibrio cholerae: The bacterium that causes cholera (SEM image) |
|
|---|---|
| ICD-10 | A00 |
| ICD-O: | |
| ICD-9 | 001 |
| OMIM | [1] |
| MedlinePlus | 000303 |
| eMedicine | med/351 |
| DiseasesDB | 2546 |
Cholera, also called Asiatic cholera or epidemic cholera, is a severe diarrheal disease that affects humans and is caused by the bacterium Vibrio cholerae.[1] Cholera is transmitted and spread to humans through consumption of water and food contaminated with the bacteria.
Cholera is a fairly preventable disease, traced to both personal and human responsibility. Contamination with the bacteria Vibrio cholerae most often occurs due to a lack of proper sanitation (clean water). Infected human feces in the water supply can spread the disease, as can crops treated with infected human feces. Certain seafood, if eaten raw or undercooked and obtained from contaminated water supplies, can contain the bacteria as well. Rarely is cholera spread by human to human contact. Both personal actions (such as good hygiene, boiling and filtering water, care regarding foods consumed, etc.) and social actions (sewage treatment, water chlorination, warnings around contaminated water sources, etc.) can prevent disease outbreaks.
Cholera is an acute illness, meaning that it has a sudden onset and a tendency to have a short course. In its most severe forms, cholera is one of the most rapidly fatal illnesses known if no treatment is provided. Fortunately, however, the cholera disease is not only preventable but also treatable with re-hydration and antibiotics.
Cholera is no longer a major health threat in the United States and other developed countries due to the enforcement of proper sanitation practices. Developing countries, on the other hand, continuously face the threat of cholera outbreaks. Referred to as a "poor man's disease," cholera is actively found in third world countries like India, Pakistan, Cambodia, and so forth. According to the World Health Organization, a single outbreak of cholera in these countries can affect anywhere from 0.2-1 percent of the local population.
The term, "cholera" is also used to refer to a variety of diseases that affect domestic animals. Characterized by severe gastroenteritis, these diseases affect animals such as hogs, chickens, and turkeys.
Symptoms
Symptoms of the cholera disease usually manifest one to three days after ingestion of contaminated food or water. Most cases of cholera are mild; however, one in 20 patients will suffer severe symptoms. Symptoms include those of the general gastrointestinal tract (GI tract), specifically upset stomach and massive, watery diarrhea. Symptoms may also include terrible muscle and stomach cramps, along with vomiting and fever in the early stages. In later stages of the disease, the diarrhea typically becomes "rice water stool" (almost clear with flecks of white) and ruptured capillaries may turn the skin black and blue. Sunken eyes and cheeks, with blue lips, are also commonly seen.
Cholera symptoms are caused by massive body fluid loss induced by the enterotoxins that V. cholerae produces. Enterotoxins are frequently cytotoxic and kill cells by altering the permeability of the epithelial cells of the intestinal wall by creating more pores in the cell membranes. V. cholerae, which produces the cholera toxin, is a Gram negative, anaerobic, rod-shaped bacterium. The enterotoxin acts on the mucosal epithelium lining of the small intestine and is responsible for the characteristic massive diarrhea of the disease.
The cholera toxin interacts with G proteins and cyclic AMP in the intestinal lining to open ion channels and alter cell permeability. As ions flow into the intestinal lumen (lining), body fluids (mostly water) flow out of the body due to the principle of osmosis. This leads to massive diarrhea as the fluid is expelled from the body. The body is "tricked" into releasing massive amounts of fluid into the small intestine. which shows up in up to 20 liters (or 20 percent of body weight) of liquid diarrhea in an adult, resulting in massive dehydration. This radical dehydration can bring death within a day through collapse of the circulatory system.
Anyone can get cholera; however, infants, children, and the elderly are more susceptible to the fatal consequences of cholera since they become dehydrated faster.
Treatment
In its most severe forms, cholera is one of the most rapidly fatal illnesses known if no treatment is provided: A healthy person may become hypotensive within an hour of the onset of symptoms and may die within 2-3 hours. More commonly, however, without rehydration treatment, which is the most common treatment method, the disease progresses from the first liquid stool to shock in 4-12 hours, with death following in 18 hours to several days.[2] Fortunately, the cholera disease is treatable. In general, patients must receive as much fluid as they lose, which can be up to twenty liters, due to diarrhea.
Treatment of cholera typically consists of aggressive rehydration to replace lost fluids and electrolytes with commercial or hand-mixed sugar-salt solutions. A 1 teaspoon (tsp) salt + 8 tsp sugar in 1 liter of clean/boiled water is commonly used. This simple and cost-effective solution created by the World Health Organization for oral rehydration has proven useful as a treatment method not only for cholera but other similar diseases. Massive injections of liquid given intravenously via an IV are used in advanced cases of dehydration. Without rehydration, the death rate can be as high as 10-50 percent, due to the serious dehydration that cholera produces.
Tetracycline antibiotics, used usually only in more severe cases, may have a role in reducing the duration and severity of cholera, although drug-resistance is beginning to occur,[3] and their effects on overall mortality are questioned.[4] Other antibiotics that have been used include ciprofloxacin and azithromycin,[5] although again, drug-resistance has now been described.[6]
Without treatment the death rate from cholera is as high as 50 percent; but with treatment, the death rate can be well below 1 percent.[7] Typical recovery time for patients is between three and six days.
Epidemiology
Prevention
Although cholera can be life-threatening, it is nearly always easily prevented, in principle, if proper sanitation practices are followed. In the United States and Western Europe, because of advanced water treatment and sanitation systems, cholera is no longer a major threat. The last major outbreak of cholera in the United States was in 1911. However, everyone, especially travelers, should be aware of how the disease is transmitted and what can be done to prevent it. Good sanitation practices, if instituted in time, are usually sufficient to stop an epidemic. There are several points along the transmission path at which the spread may be halted:
- Sickbed: Proper disposal and treatment of the germ infected fecal waste (and all clothing and bedding that come in to contact with it) produced by cholera victims is of primary importance.
- Sewage: Treatment of general sewage before it enters the waterways or underground water supplies prevent possible undetected patients from spreading the disease.
- Sources: Warnings about cholera contamination posted around contaminated water sources with directions on how to decontaminate the water.
- Sterilization: Boiling, filtering, and chlorination of water kills the bacteria produced by cholera patients and prevents infections, when they do occur, from spreading. Water filtration, chlorination, and boiling are by far the most effective means of halting transmission. All materials (clothing, bedding, etc.) that come in contact with cholera patients should be sterilized in hot water using (if possible) chlorine bleach. Hands and other parts that touch cholera patients or their clothing, and so forth, should be thoroughly cleaned and sterilized. All water used for drinking, washing, or cooking should be sterilized by boiling, chlorination, or use of iodine tablets in any area where cholera may be present. Cloth filters, though very basic, have greatly reduced the occurrence of cholera when used in poor villages in Bangladesh that rely on untreated surface water.
- Food consumption: Minimize consumption of raw foods like oysters and shellfish, especially those that originate from coastal waters, where cholera naturally exists. Eat cooked foods and eat them while they are hot. Concentrate on eating fruits with thick, intact skin that has to be peeled before consumption.
In general, public health education and good sanitation practices are the limiting factors in preventing transmission.
A vaccine is available for travelers and residents of areas where cholera is known to be an active threat. Unfortunately, it is not very effective. Currently, the United States Center for Disease Control and Prevention (CDCP) does not recommend the vaccine for travelers, since it, at most, provides 25-50 percent immunity against the disease for a maximum of up to six months. The practice of proper sanitation methods and common precautions discussed above are advised.
Susceptibility
Recent epidemiological research suggests that an individual's susceptibility to cholera (and other diarrheal infections) is affected by their blood type: Those with type O blood are the most susceptible,[8] while those with type AB blood are the most resistant.
About one million V. cholerae bacteria must typically be ingested to cause cholera in normally healthy adults, although increased susceptibility may be observed in those with a weakened immune system, individuals with decreased gastric acidity (as from the use of antacids), or those who are malnourished. V. cholerae are sensitive to acid, and the stomach's acidic environment serves as the first line of defense against the cholera disease. Decreased acidity due to a weak immune system or use of medications that decrease or block acid production in the stomach promote V. cholerae survival and cause more severe symptoms of the disease.
It has also been hypothesized that the cystic fibrosis genetic mutation has been maintained in humans due to a selective advantage: Heterozygous carriers of the mutation (who are thus not affected by cystic fibrosis) are more resistant to V. cholerae infections.[9] In this model, the genetic deficiency in the cystic fibrosis transmembrane conductance regulator channel proteins interferes with bacteria binding to the gastrointestinal epithelium, thus reducing the effects of an infection.
Transmission
Cholera is rarely spread directly from one person to another, but rather through the fecal-oral route. Persons infected with cholera endure massive diarrhea. This highly liquid diarrhea, which is often compared to "rice water," is loaded with bacteria that can spread under unsanitary conditions, to infect water sources used by other people. Cholera is transmitted through population centers by the ingestion of feces-contaminated water that is loaded with the cholera bacterium. The source of the contamination is typically other cholera patients. When their untreated diarrhea discharge is allowed to get into waterways, groundwater, or the drinking water supply, the bacteria spreads easily and rapidly.
Also, any infected water and any foods washed in the water can cause an infection. Shellfish populations living in the affected waterway is a common example. V. cholerae occurs naturally in the plankton of fresh, brackish (water that is saltier than fresh water, but not as salty as seawater), and salt waters, attached primarily to copepods in the zooplankton. Both toxic and non-toxic strains exist. Non-toxic strains, however, can acquire toxicity through a lysogenic bacteriophage.[10] Coastal cholera outbreaks typically follow algal blooms. This makes cholera a zoonosis, or an infectious disease that is able to be transmitted from one type of animal to another, or from animals, both wild and domestic, to humans.
Biochemistry of the V. cholerae bacterium
Most of the V. cholerae bacteria in the contaminated water that a potential host drinks do not survive the very acidic conditions of the human stomach.[11] But the few bacteria that manage to survive the stomach's acidity conserve their energy and stored nutrients during the perilous passage through the stomach by shutting down much of their protein production. When the surviving bacteria manage to exit the stomach and reach the favorable conditions of the small intestine, they need to propel themselves through the thick mucus that lines the small intestine in order to get to the intestinal wall where they can thrive. So they start up production of the hollow cylindrical protein flagellin in order to make flagella, the curly whip-like tails that the bacteria rotate to propel themselves through the pasty mucus that lines the small intestine.
Once the cholera bacteria reach the intestinal wall, they do not need the flagella propellers to move themselves any more. Responding to the changed chemical surroundings, they stop producing the protein flagellin and again conserve energy and nutrients by changing the mix of proteins that they manufacture. On reaching the intestinal wall, the bacteria start producing the toxic proteins that give the infected person a watery diarrhea, which carries the multiplying and thriving new generations of V. cholerae bacteria out into the drinking water of the next host—if proper sanitation measures are not in place.
Microbiologists have studied the genetic mechanisms by which the V. cholerae bacteria turn off the production of some proteins and turn on the production of other proteins as they respond to the series of chemical environments they encounter, passing through the stomach, through the mucous layer of the small intestine, and on to the intestinal wall.[12] Of particular interest have been the genetic mechanisms by which cholera bacteria switch on the protein production of the toxins that interact with host cell mechanisms which then pump chloride ions into the small intestine, creating an ionic pressure which prevents sodium ions from entering the cell. The choride and sodium ions create a salt water environment in the small intestines through which osmosis can pull up to 20 liters of water through the intestinal cells, which then creates the massive amounts of diarrhea. The host can become rapidly dehydrated if an appropriate mixture of dilute salt water and sugar is not taken to replace the blood's water and salts lost in the diarrhea.
By inserting separately successive sections of V. cholerae DNA into the DNA of other bacteria, such as E. coli, that would not naturally produce the protein toxins, researchers were able to find out the separate pieces of the mechanisms by which V. cholerae respond to the changing chemical environments of the stomach, mucous layers, and intestinal wall. Researchers discovered that a complex cascade of regulatory proteins exists that controls the expression of V. cholerae virulence determinants. In responding to the chemical environment at the intestinal wall, the V. cholerae bacteria produce the TcpP/TcpH proteins which, together with the ToxR/ToxS proteins, activate the expression of the ToxT regulatory protein. ToxT then directly activates expression of virulence genes that produce the toxins that cause diarrhea in the infected person and that permit the bacteria to colonize the the infected intestine. Current research aims at discovering "the signal that makes the cholera bacteria stop swimming and start to colonize (that is, adhere to the cells of) the small intestine."[13]
History
Origin and spread
Cholera was originally endemic to the Indian subcontinent, with the Ganges River likely serving as a contamination reservoir. It spread by trade routes (both land and sea) to Russia, then to Western Europe, and then from Europe to North America. It is now no longer considered an issue in Europe and North America, due to water filtration and chlorination of the water supply.
- 1816-1826: First Cholera pandemic: Previously restricted, the pandemic began in Bengal, India, then spread across the rest of India by 1820. It extended as far as China and the Caspian Sea before receding.
- 1829-1851: Second Cholera pandemic: The disease reaches Europe, including London and Paris in 1832. In London, it claimed 6,536 victims; in Paris, 20,000 succumbed (out of a population of 650,000) with about 100,000 deaths in all of France. It reached Russia (Cholera Riots), Quebec and Ontario (Canada), and New York in the same year, moving all the way to the Pacific coast of North America by 1834.
- 1849: Second major outbreak in Paris. In London, it was the worst outbreak in the city's history, claiming 14,137 lives. The outbreak reportedly started when a sailor in Southwark was diagnosed with the disease on September 22, 1848. The outbreak continued on well into 1849.[14] The outbreak also claimed 5,308 lives in the port city of Liverpool, England, and 1,834 in Hull, England. An outbreak in North America took the life of former U.S. President James K. Polk. Cholera spread throughout the Mississippi River system, killing over 4,500 in St. Louis, over 3,000 in New Orleans, and thousands in New York[15] In 1849, cholera was spread along the California and Oregon trail as hundreds died on their way to Utah, Oregon, and the California Gold Rush.[16]
- 1852-1860: Third Cholera pandemic: Mainly affected Russia, with over a million deaths. In 1853-4, London's epidemic claimed 10,738 lives.
- 1854: Outbreak of cholera in Chicago took the lives of 1,424 people.[17] The Soho outbreak in London was stopped by removing the handle of the Broad Street pump by a committee instigated to action by physician John Snow.[18]
- 1863-1875: Fourth Cholera pandemic: Spread mostly in Europe and Africa.
- 1866: Outbreak in North America. In London, a localized epidemic in the East End claimed 5,596 lives just as London was completing its major sewage and water treatment systems—the East End was not quite complete. William Farr, using the work of John Snow (physician) et. al. regarding contaminated drinking water being the likely source of the disease, was able to relatively quickly identify the East London Water Company as the source of the contaminated water. Quick action prevented further deaths.[19]
- 1881-1896: Fifth Cholera pandemic: The 1892 outbreak in Hamburg, Germany, was the only major European outbreak; about 8,600 people died in Hamburg, causing a major political upheaval in Germany, as control over the city was removed from a city council that had not updated Hamburg's water supplies. This was the last serious European cholera outbreak.
- 1899-1923: Sixth Cholera pandemic: This pandemic had little effect in Europe because of advances in public health, but Russia was badly affected again.
- 1961-1970s: Seventh Cholera pandemic: It began in Indonesia, called El Tor after the strain, and reached Bangladesh in 1963, India in 1964, and the USSR in 1966. From North Africa, it spread into Italy by 1973. In the late 1970s there were small outbreaks in Japan and in the South Pacific. There were also many reports of a cholera outbreak near Baku in 1972, but information of this was suppressed in the Soviet Union. This pandemic eventually reached Latin America in 1991. There were 400,000 reported cases and 4,000 deaths in 16 countries of the Americas that year alone.
- January 1991 to September 1994: Outbreak in South America, apparently initiated by ship-discharged water. Beginning in Peru, there were 1.04 million identified cases and almost 10,000 deaths. The causative agent was an O1, El Tor strain, with small differences to the seventh pandemic strain. In 1992, a new strain appeared in Asia, a non-O1, nonagglutinable vibrio (NAG) named O139 Bengal. It was first identified in Tamilnadu, India and for a while displaced El Tor in southern Asia before decreasing in prevalence from 1995, to around 10 percent of all cases. It is considered to be an intermediate between El Tor and the classic strain and occurs in a new serogroup. There is evidence as to the emergence of wide-spectrum resistance to drugs such as trimethoprim, sulfamethoxazole, and streptomycin.
False report of cholera
A persistent myth states that the 1885 epidemic in Chicago killed 90,000 people from cholera and typhoid fever. This story has no factual basis. In 1885, there was a torrential rainstorm that flushed the Chicago river and its attendant pollutants into Lake Michigan far enough that the city's water supply was contaminated. Fortunately, cholera was not present in the city and this is not known to have caused any deaths. It did, however, cause the city to become more serious about their sewage treatment.
Other historical information
In the past, people traveling in ships would hang a yellow flag if one or more of the crew members suffered from cholera. Boats with a yellow flag hung would not be allowed to disembark at any harbor for an extended period of time, typically 30 to 40 days.[20]
Famous cholera victims
Cholera has claimed the lives of several well known people over its long history. Some were positively affected by the disease while others have only been speculated to have passed away due to cholera. For example, the crying and pathos in the last movement of Pyotr Ilyich Tchaikovsky's last symphony made people think that Tchaikovsky had a premonition of death. "A week after the premiere of his Symphony No. 6 (Tchaikovsky)(Sixth Symphony), Tchaikovsky was dead—6 Nov. 1893. The cause of this indisposition and stomach ache was suspected to be his intentionally infecting himself with cholera by drinking contaminated water. The day before while having lunch with Modest Tchaikovsky (his brother and biographer), he is said to have poured faucet water from a pitcher into his glass and drunk a few swallows. Since the water was not boiled and cholera was once again rampaging Saint Petersburg, Russia, such a connection was quite plausible …."[21]
Other famous people who succumbed to the cholera disease include:
- James K. Polk, ex-President of the United States
- Mary Abigail Fillmore, daughter of ex-U.S. president Millard Fillmore
- Elliott Frost, son of American poet Robert Frost
- Nicolas Léonard Sadi Carnot, French physicist responsible for such concepts as Carnot efficiency, Carnot theorem, Carnot heat engine, and others
- Georg Wilhelm Friedrich Hegel, considered one of the representatives of German idealism
- Samuel Charles Stowe, son of Harriet Beecher Stowe
- Carl von Clausewitz, Prussian soldier famous for his military treatise, Vom Kriege
- George Bradshaw, originator of the railway timetable
- Adam Mickiewicz, Polish poet and writer
- August von Gneisenau, Prussian field marshal
- William Jenkins Worth, U.S. general during the Mexican-American War
- John Blake Dillon, one of the founding members of the Young Ireland movement
- Daniel Morgan Boone, founder of Kansas City, Missouri and son of Daniel Boone
- James Clarence Mangan, Irish poet
- Mohammad Ali Mirza, Dowlatshahi of Persia
- Ando Hiroshige, Japanese ukiyo-e woodblock print artist
- Juan de Veramendi, Mexican Governor of Texas and father-in-law of Jim Bowie
- Grand Duke Constantine Pavlovich of Russia
- William Shelley, son of Mary Shelley
- William Godwin, father of Mary Shelley
- Judge Daniel Stanton Bacon, father-in-law of George Armstrong Custer
- Inessa Armand, mistress of Lenin and the mother of his son, Andre
- Honinbo Shusaku, famous Go (East Asian board game) player renowned for his play
Alexandre Dumas, père, French author of The Three Musketeers and The Count of Monte Cristo, also contracted cholera in the 1832 Paris epidemic and almost died, before he wrote these two novels.
Research
The major contributions to fighting cholera were made by physician and self-trained scientist John Snow (1813-1858), who found the link between cholera and contaminated drinking water in 1854, and also by Henry Whitehead, an Anglican minister, who helped John Snow track down and verify the source of the disease, an infected well in London. Their conclusions and writings were widely distributed and firmly established for the first time a definite link between germs and disease. Clean water and good sewage treatment, despite their major engineering and financial cost, slowly became a priority throughout the major developed cities in the world from this time onward. Robert Koch, 30 years later in 1885, identified V. cholerae with a microscope as the bacillus causing the disease. The bacterium had been originally isolated thirty years earlier (1855) by Italian anatomist Filippo Pacini, but its exact nature and his results were not widely known around the world.
Cholera has been used in the laboratory for the study of the evolution of virulence.
Notes
- ↑ K.J. Ryan and C.G. Ray (eds.), Sherris Medical Microbiology (McGraw Hill, 2004, ISBN 0838585299).
- ↑ K. McLeod, Our sense of Snow: John Snow in medical geography," Social Science and Medicine 50(7-8): 923-935 (PubMed, 2000). Retrieved February 27, 2017.
- ↑ S. K. Bhattacharya, "An evaluation of current cholera treatment." Expert Opin Pharmacother 4(2): 141-6 (PubMed, 2003). Retrieved February 27, 2017.
- ↑ V. K. Parsi, "Cholera," Prim. Care Update Ob Gyns 8(3): 106-109 (PubMed, 2001). Retrieved February 27, 2017.
- ↑ D. Saha et al., "Single dose azithromycin for the treatment of cholera in adults," New England Journal of Medicine 354(23): 2452–2462. (2006).
- ↑ B. V. S. Krishna, A. B. Patil, and M. R. Chandrasekhar, "Fluoroquinolone-resistant Vibrio cholerae isolated during a cholera outbreak in India," Trans R Soc Trop Med Hyg 100(3): 224-226 (2006).
- ↑ D. Sack, R. Sack, G. Nair, and A. Siddique, "Cholera," Lancet 363(9404): 223-33 (PubMed, 2004). Retrieved February 27, 2017.
- ↑ D. Swerdlow, E. Mintz, M. Rodriguez, E. Tejada, C. Ocampo, L. Espejo, T. Barrett, J. Petzelt, N. Bean, and L. Seminario, "Severe life-threatening cholera associated with blood group O in Peru: Implications for the Latin American epidemic," Journal of Infectious Diseases 170(2): 468-72 (PubMed, 1994). Retrieved February 27, 2017.
- ↑ J. Bertranpetit and F. Calafell, "Genetic and geographical variability in cystic fibrosis: evolutionary considerations," Ciba Foundation Symposium 197: 97-114; discussion 114-118 (PubMed, 1996). Retrieved February 27, 2017.
- ↑ BMJ Publishing Group Ltd and Royal College of Paediatrics and Child Health, "Cholera phage discovery," Archives of Disease in Childhood Online 76: 274 (1997). Retrieved February 27, 2017.
- ↑ L. H. Hartwell, L. Hood, M. L. Goldberg, A. E. Reynolds, L. M. Silver, and R. C. Veres, Genetics: From Genes to Genomes, p.551-2, 572-4 (Boston: Mc-Graw Hill, 2006, ISBN 0073227382).
- ↑ V. DiRita, C. Parsot, G. Jander, and J. Mekalanos, "Regulatory cascade controls virulence in Vibrio cholerae," Proceedings of the National Academy of Sciences of the United States of America 88(12): 5403-5407 (PubMed, 1991). Retrieved February 27, 2017.
- ↑ Hartwell, p. 574.
- ↑ P. Bingham, N. Q. Verlander, and M. J. Cheal, "John Snow, William Farr and the 1849 outbreak of cholera that affected London: A reworking of the data highlights the importance of the water supply," Journal of the Royal Institute of Public Health 118: 387-394 (2004). Retrieved February 27, 2017.
- ↑ C. E. Rosenberg, The Cholera Years: The United States in 1832, 1849, and 1866 (The University of Chicago Press, 1987, ISBN 978-0226726779).
- ↑ Utah Academic Library Consortium, "Trails of hope: Overland diaries and letters, 1846-1869, Utah Academic Library Consortium. Retrieved February 27, 2017.
- ↑ Encyclopedia of Chicago, Epidemics Retrieved February 27, 2017.
- ↑ John Snow, "On the mode of communication of cholera," Edinburgh Medical Journal 1: 668-670 (1855-56). Retrieved February 27, 2017.
- ↑ S. Johnson, The Ghost Map (Riverhead Hardcover, 2006, ISBN 978-1594489259), 209.
- ↑ Philip A. Mackowiak and P. Sehdev, "The origin of quarantine," Clinical Infectious Diseases 35: 1071-1072 (Infectious Diseases Society of America, 2002). Retrieved February 27, 2017.
- ↑ A. Neumayr, Music and Medicine: Chopin, Smetana, Tchaikovsky, Mahler: Notes on Their Lives, Works, and Medical Histories (Medi-Ed Press, 1997, ISBN 978-0936741086), 282-283.
References
ISBN links support NWE through referral fees
- Hartwell, L. H., L. Hood, M. L. Goldberg, A. E. Reynolds, L. M. Silver, and R. C. Veres. Genetics: From Genes to Genomes. Boston: Mc-Graw Hill, 2006. ISBN 0073227382
- Johnson, S. The Ghost Map. Riverhead Hardcover, 2006. ISBN 978-1594489259
- Neumayr, A. Music and Medicine: Chopin, Smetana, Tchaikovsky, Mahler: Notes on Their Lives, Works, and Medical Histories. Medi-Ed Press, 1997. ISBN 978-0936741086
- Rosenberg, C. E. The Cholera Years: The United States in 1832, 1849, and 1866. The University of Chicago Press, 1987. ISBN 978-0226726779
- Ryan, K.J., and C.G. Ray (eds.). Sherris Medical Microbiology. McGraw Hill, 2004. ISBN 0838585299
External links
All links retrieved February 16, 2017.
- Cholera - World Health Organization.
- Cholera - Centers for Disease Control and Prevention.
- Steven Shapin, Sick City: Maps and mortality in the time of cholera, (The New Yorker, Nov 2006).
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
- Cholera history
- Enterotoxin history
- Zoonosis history
- Lazare_Carnot history
- Georg_Wilhelm_Friedrich_Hegel history
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
↧ Download as ZWI file | Last modified: 02/04/2023 03:44:17 | 45 views
☰ Source: https://www.newworldencyclopedia.org/entry/Cholera | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed:

 KSF
KSF