Tuskegee Syphilis Study
 From Nwe
From Nwe The Tuskegee Syphilis Study (1932-1972), officially titled "The Tuskegee Study of Untreated Syphilis in the Negro Male," was a forty-year, observational research endeavor funded by the U.S. Public Health Service (USPHS) that is infamous as a case of unethical human subject research. The study participants included six hundred African American men of low educational and socioeconomic levels in Macon County, Alabama, with an initial group of 399 with syphilis and 201 later added as a control population. The goal was to evaluate the natural course of syphilis, a serious, sexually transmitted bacterial disease, while foregoing treatment, with the endpoint (after modification of the original short-term timeframe) including up to death and postmortem evaluation. Enrollment began in October 1932. The exposure of this study in July 1972 by Associated Press reporter Jean Heller led to a public outcry and the termination of the study the same year.
Numerous unethical actions — including lack of informed consent, use of a vulnerable population, deception, and withholding treatment— make the Tuskegee Syphilis Study one of the most notorious chapters in human subject research. For example, the men serving as subjects were not properly informed about the study in which they were asked to volunteer, with outright deception used in enrolling the men and keeping them in the study. A particularly well-known and scandalous aspect of the study was the effort made to deprive the men of treatment for the disease. There were treatments available from the start of the study, albeit those carried significant risks. However, by the time of World War II, penicillin, which offered a very effective treatment, was being mass produced and became widely available for civilian populations after the war, including being used for those with syphilis in Macon Country. However, penicillin was withheld from those in the study, with other physicians and agencies persuaded to aid in that effort, resulting in serious health complications (organ damage, blindness, mental impairment, etc.) and death of study subjects, the spreading of the disease to sexual partners, and children born with congenital syphilis.
The revelations of the unethical actions in this study became a milestone as it catalyzed efforts to address the ethics of human subject research, including Congressional hearings and the formulation of the Belmont Report and the Common Rule. The Tuskegee Syphilis Study also has been cited as an example of racism and the "Tuskegee Effect" as deterring participation of African-Americans in medical research and fostering distrust of the health-care system.
The Study
Overview
The research study is officially titled "the Tuskegee Study of Untreated Syphilis in the Negro Male," although it is commonly referred to as the Tuskegee Syphilis Study, the Tuskegee Experiment, the Tuskegee Study, or the Tuskegee Study of Untreated Syphilis (TSUS).
The study was sponsored by a United States agency, the U.S. Public Health Service (USPHS). Other organizations that were involved at various times included the Tuskegee Institute (now Tuskegee University, a historically Black land-grant university in Tuskegee, Alabama), the Alabama State and Macon County Boards of Health, the Tuskegee Veteran's Affairs Hospital (originally set up to provide long-term care for African-American veterans from World War I), John A. Andrew Memorial Hospital (founded as the first Black hospital in Alabama, which closed in 1987, but later reopened as the National Center for Bioethics in Research and Healthcare), the Milbank Memorial Fund, various local Black churches and public schools, and plantation owners (Thomas and Crouse Quinn 1991; Baker et al. 2005).
It was originally planned to last for six to eight months, but was extended to a long-term study, running from 1932 to 1972. The groundwork for the study began in 1929, enrollment began in 1932, there was a public outcry in 1972 after exposure in a July 25 Associated Press article (which also landed on the front page of the New York Times on July 26), an ad hoc advisory panel convened and made their recommendation to terminate the program, and the Assistant Secretary for Health called for it to be terminated in November of 1972. In March of 1973 treatment was authorized. The forty-year time span of the study has been cited as "longest nontherapeutic experiment on human beings in medical history" (Tomas and Crouse Quinn 1991) and "longest observational study in medical history" (Baker et al. 2005).
Syphilis and the Foundation for the Study
Syphilis
Syphilis is a sexually transmitted disease (STD) that is caused by the bacterium Treponema pallidum. It can have serious health complications when left untreated, including organ damage, blindness, dementia, and death.
Syphilis is commonly spread by direct contact with a syphilis sore during sex (vaginal, anal, or oral), with sores found on the penis, vagina, anus, rectum, lips, or mouth. But, since it involves the bacterium entering the body through cuts or abrasions in one's skin or mucous membrane, it also can spread, although less commonly, by other means of unprotected, close contact with an active lesion, such as during kissing. It is not spread by use of the same toilet, bathtub, clothing, or swimming pool with an infected person.
Syphilis is commonly divided into four stages: primary, secondary, latent, and tertiary.
- Primary syphilis generally exhibits with a sore or sores at the site of original infection, such as around the genitals, anus, or mouth. Such sores are commonly painless and may go unnoticed, with the sores commonly lasting from three to six weeks; these symptoms will eventually disappear regardless of treatment. However, without treatment, the infection can move to the second stage, secondary syphilis.
- Secondary syphilis can include such symptoms as a skin rash, mucous membrane lesions, fever, sore throat, swollen lymph nodes, headaches, and/or fatigue. The rash could cover one's entire body, including the soles of the feet and palms of the hands. Again, the symptoms from this stage will eventually disappear with or without treatment, but without treatment will move to the latent and possibly tertiary stages.
- Latent stage syphilis exhibits no visible signs or symptoms. A person may stay in the stage for years without the symptoms, but without treatment the syphilis remains in the body and can transition to tertiary syphilis.
- Tertiary syphilis is the stage associated with severe medical complications and can affect various organs and systems, including the heart, blood vessels, brain, and nervous system. Not all people who have syphilis transition to tertiary syphilis during their lifetime, but when it happens, often ten to thirty years after the initial infection, then it is very serious, with organ damage and possibly death.
The stages may overlap, and symptoms do not always occur in the same order. Syphilis is contagious during its primary and secondary stages; it sometimes is contagious in the early latent period as well.
Syphilis can spread to the brain and nervous system during any of the stages; it is then known as neurosyphilis. Patients with neurosyphilis may experience difficulty in coordination, paralysis, severe headaches, and dementia. Syphilis can also spread to the eye during any of these stages, and then is known as ocular syphilis. Patients with ocular syphilis may experience vision changes or blindness. Syphilis can also be spread to a mother's baby if she is infected during pregnancy, being transmitted through the placenta or during birth; a baby born with this condition is said to have congenital syphilis.
Syphilis in Macon County, Alabama
The origins of the Tuskegee Syphilis Study trace to 1929, when the USPHS, with the aid of a grant from the Julius Rosenwald Fund, began a study to determine the prevalence of syphilis among Blacks in the rural south and the feasibility of mass treatment. The study ran until 1931 and focused on six counties in the South. Macon County was found to have the highest syphilis rates among the counties studied (Brandt 1978; Thomas and Crouse Quinn 1991; Baker et al. 2005; Clark 1932).
In this 1929-1931 study, more than one-third of residents tested in Macon County were found to be syphilitic. Thomas and Crouse Quinn (1991) report this syphilis control demonstration project "found that in Macon County, Alabama, 35% to 40% of all age groups tested were positive for syphilis." Dr. Traliaferro Clark, who was chief of the USPHS Venereal Disease Division, and who authored the Rosenwald Study Report (The Control of Syphilis in Southern Rural Areas, 1932), wrote that approximately 35% of the those examined in the county were syphilitic. Baker et al. (2005) further note that "during the 1920s, 36% of the 27,000 residents of Tuskegee, Macon County, Alabama were infected with syphilis, given this place a syphilis prevalence among the greatest in the United States."
When a study was conceived to understand medical deterioration over time due to syphilis, the prevalence in Macon County was cited as reason for this area to be a natural site to do the observations. Thus, the Tuskegee Study of Untreated Syphilis came about. Note that the Rosenwald Study, in addition to ascertaining the prevalence of syphilis, also "concluded that mass treatment could be successfully implemented among rural Blacks," but this part of the study was ignored (Brandt 1978).
There were treatments available at the time this study was conceived, such as use of arsphenamine, bismuth, iodide and arsenic, and they had some limited effectiveness, such as reducing the progression of latent syphilis to tertiary syphilis. However, these treatments also carried significant risks (Baker et. al, 2005; Paul and Brookes 2015). On this basis, there was a rationalization proposed by the study architects for observing the progression of syphilis without treatment.
Brandt (1978) noted that "from its inception, the USPHS regarded the Tuskegee Study as a classic 'study in nature' rather than an experiment." He further noted regarding Dr. Taliaferro Clark, chief of the USPHS Venereal Disease Division at the start of the study in 1929, "as long as syphilis was so prevalent in Macon and most of the Blacks went untreated throughout life, it seemed only natural to Clark that it would be valuable to observe the consequences."
The study
The goal of the study was to observe medical deterioration over time of men with untreated syphilis. Enrollment began in October 1932. From over 4,000 men in Macon County screened for syphilis, a total of 399 men with positive serology were enrolled. The enrollees were African-American men of low educational and socioeconomic status — largely indigent, African-American sharecroppers and tenant farmers. Then men were informed they had "bad blood" and enticed with such incentives as medical care, free lunches, free medicine (for diseases other than syphilis), and free transportation to and from hospitals. They did receive medical follow-up in terms of physical examinations, lumbar punctures, and blood tests, but only a few were specifically treated for syphilis with bismuth and arsenicals. Rather, they were informed that their "bad blood" could be treated by such things as vitamins, aspirins, and tonics, which were provided free by the researchers (Baker et al. 2005; Heller 1972).
The initial conception of the study was a program that would run for six to eight months. However, during the course of that time, the six- to eight-month timeframe was judged too brief for the study, and thus it was extended to an endpoint of death and autopsies, with free burial after autopsies added as an incentive. In addition a control group was added with 201 men without a positive serology for syphilis (Baker et al. 2005). Brandt (1978) noted "control subjects who became syphilitic were simply transferred to the test group — a strikingly inept violation of standard research protocol."
One of the key persons employed throughout the 40-year study was Eunice Rivers, a Black public health nurse from Macon County, who was a primary contact person for the subjects. She provided transportation, offered reassurance, dispensed medicine (non-effective medicine such as aspirin and "spring tonic"), and organized the subjects for examinations, as well as secured approval from the men or their families to perform autopsies.
When the United States entered into World War II, the researchers was able to gain the cooperation of the Macon County draft board to decline conscription of those enrolled in the study in order to not disrupt the study (Baker et al. 2005).
Penicillin, an antibiotic whose discovery is usually attributed to Scottish scientist Alexander Fleming in 1928 at his laboratory in St. Mary's Hospital in London (others had earlier noted the antibacterial effects of the fungus Penicillium) does offer a very effective treatment of syphilis. Penicillin began to be mass produced during World War II for the troops, and after the war, in 1945, became available to the general U.S. public. By 1947, it was widely used to treat syphilis, and the USPHS began to administer it to syphilis patients, including those in Macon County. However, it was withheld from those in the study (Baker et al. 2005).
In 1964, the Declaration of Helsinki was issued by the World Health Organization to guide ethics in medical research. The Tuskegee Syphilis Study violated key provisions of the Declaration of Helsinki, such as informed consent of the subjects. However, it was not used to halt the study, which continued until a public outcry in 1972 as a result of awareness of the project spurred by an Associated Press article.
Over 100 participants died of syphilis or its complications during the course of the study and many wives and girlfriends contracted the disease from the study participants. The number of children born with congenital syphilis is not known (Baker et al. 2005).
Investigations, public outcry, and ending of the study
There were a number of individuals who expressed reservations about the ethics of the study. One of these was Peter Buxton, who was working as a venereal disease interviewer and investigator with the USPHS in San Francisco. In November of 1966, he sent a letter to the Centers for Disease Control (CDC) in Atlanta, Georgia — specifically to the CDC's Director of the Division of Venereal Diseases, Dr. William J. Brown — to relay his moral concerns about the study and to inquire whether any of the men had been told the nature of the study and whether any had received proper medical treatment. Two years later, in November of 1968, he wrote a second time to Dr. Brown in which he stated: "I have grave moral doubts as to the propriety of this study." He also expressed his concern about the racial component of the study participants and the appearance this gave in terms of African-Americans being used for medical experiments (Thomas and Crouse Quinn 1991).
Dr. William Brown brought this letter to the Director of the Centers for Disease Control. In February of 1969, the CDC convened a panel to review and discuss the Tuskegee Syphilis Study. The panel decided against treating the men and recommended it continue until its "end point." The panel further recommended that the study be upgraded scientifically.
When the CDC failed to address his concerns, Buxton leaked the story to a reporter with the Associated Press, Jean Heller, who published on July 25, 1972, an article titled: "Syphilis Victims in U.S. Study Went Untreated for 40 years," which ran in the Washington Star (Thomas and Crouse Quinn 1991). The following day, on July 26, the New York Times published this story on its front page, and it became the subject of editorials across the United States.
Among statements in Heller's article were the following, with the first one being the lead sentence (Heller 1972):
- For 40 years the United States Public Health Service has conducted a study in which human beings with syphilis, who were induced to serve as guinea pigs, have gone without medical treatment for the disease and a few have died of its late effects, even though an effective therapy was eventually discovered.
- The experiment, called the Tuskegee Study, began in 1932 with about 600 black men, mostly poor and uneducated, from Tuskegee, Ala., an area that had the highest syphilis rate in the nation at the time.
- The Tuskegee Study began 10 years before penicillin was found to be a cure for syphilis and 15 years before the drug became widely available. Yet, even after penicillin became common, and while its use probably could have helped or saved a number of the experiment subjects, the drug was denied them.
- Members of Congress reacted with shock to the disclosure today that the syphilis experimentation on human guinea pigs had taken place.
- Senator William Proxmire...called the study "a moral and ethical nightmare.
Heller further noted that the Assistant Secretary of Health, Education and Welfare for Health and Scientific Affairs, Dr. Merlin DuVal, "expressed shock on learning of the study. He said that he was making an immediate investigation."
The study was widely denounced nationwide, including in many newspaper editorials. Those denouncing the Tuskegee Syphilis Study included officials of the Department of Health, Education, and Welfare (HEW). (The Department of Health, Education, and Welfare would become in 1979 two separate agencies, the Department of Health and Human Services, or HHS, and Department of Education.) Dr. Donald Printz, an official of the CDC's Venereal Disease Branch, publicly stated the Tuskegee Study was "almost like genocide...a literal death sentence was passed on some of those people" (Thomas and Crouse Quinn 1991). On the other hand, Dr. William J. Brown, mentioned above as the person to which Buxton had written, is quoted in an August 9, 1972, article in the New York Times as explaining the reason for the CDC's 1969 panel's recommendation to continue the study was because it was believed the syphilis in the survivors was dormant and treatment would do more harm than good. He is quoted as stating the following (New York Times August 8, 1972):
I do know why we made the decision we did in 1968 and 1969. When a person has had syphilis as long as the men were were dealing with at that time and the disease has no serious side effects, the chances are excellent that it never will. We made our decision based on the knowledge that therapy in the late 1960's would very probably do more damage than good.
In response to the light shed on this study, the Department of Health, Education, and Welfare formed a panel in August 1972 to investigate, focusing on informed consent and penicillin as a treatment. The nine-member panel included representatives of medicine, law, education, health administration, labor, religion, and public affairs (Paul and Brookes 2015). The panel focused on (1) whether the study was justified in 1932 and whether the men had given informed consent; (2) whether the men should have been given penicillin when it became publicly available, and (3) whether the study should be terminated (Brandt 1978).
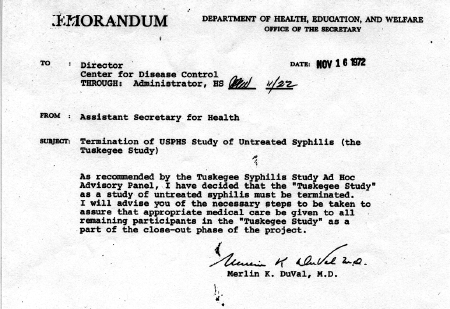
The conclusion of the panel was the study was ethically unjustified. Dr. DuVal, in a November 14, 1972, memorandum stated:
As recommended by the Tuskegee Syphilis Study Ad Hoc Advisory Panel, I have decided that the "Tuskegee Study" as a study of untreated syphilis must be terminated. I will advise you of the necessary steps to be taken to assure that appropriate medical care be given to all remaining participants in the "Tuskegee Study" as a part of the close-out phase of the project.
In March 1973, treatment was authorized for the study participants (Baker et al. 2005).
The panel's report was issued in April 1973 (Paul and Brookes 2015). The following is a quote from the HEW Final Report (Brandt 1978):
In retrospect, the Public Health Service Study of Untreated Syphilis in the Male Negro in Macon Country, Alabama was ethically unjustified in 1932. This judgement made in 1973 about the conduct of the study in 1932 is made with the advantage of hindsight acutely sharpened over some forty years, concerning an activity in a different age with different social standards. Nevertheless, one fundamental ethical rule is that a person should not be subjected to avoidable risk of death or physical harm unless he freely and intelligently consents. There is no evidence that such consent was obtained from the participants in the study.
Brandt (1978) found issue with the Final Report..
Implicit was the assumption that no adequate therapy existed prior to penicillin. Nonetheless, medical authorities firmly believed in the efficacy of arsenotherapy for treating syphilis at the time of the experiment's inception in 1932. The panel further failed to recognize that the entire study had been predicated on nontreatment. Provision of effective medication would have violated the rationale of the of the experiment — to study the natural course of the disease until death....The other focus of the Final Report —informed consent— also served to obscure the historical facts of the experiment....The Final Report's statement "Submitting voluntarily is not informed consent" indicated that the panel believed that the men had volunteered for the experiment. The records in the National Archives make clear that the men did not submit voluntarily to an experiment; they were told and they believed that they were getting free treatment from expert government doctors for a serious disease.
Ethical Failings
The Tuskegee Syphilis Study was set up to follow the natural progression of "untreated syphilis" in the men enrolled; that is, documenting the deterioration of the men over time while withholding treatment. In 1932, the justification for beginning the research was that such an important study could yield many benefits in terms of knowledge about this serious disease. Another justification by the researchers was that they considered the existing treatments to not be highly effective and to carry significant risks. However, it is clear that even in the very beginning of the study, there were disturbing ethical failings. These were then magnified when an effective treatment was found and yet denied to the participants — including via some extraordinary efforts — for the sake of not impacting the study. Even after codes of ethics for medical research were developed and gained prominence, such as the Nuremberg Code and the Declaration of Helsinki, the researchers continued violating basic ethical standards for conducting research with human subjects.
Among the ethical transgressions were manipulation of a vulnerable population, lack of informed consent, deception, withholding of treatment, undue influence, and racism.
Use of a vulnerable population
The population chosen for this study was a highly vulnerable sector of American society: indigent, African-American sharecroppers and tenant farmers who were living with syphilis and in many cases were illiterate. Thomas and Crouse Quinn (1991) noted: "The fact that Whites ruled Blacks in Macon County, coupled with the Black men's extreme poverty and almost total lack of access to health care, made the men willing subjects."
The Belmont Report, which was developed partly in response to the Tuskegee Syphilis Study, addresses this issue in one of its three core principles, that of "Justice." This principle requires the protection of vulnerable subjects from selection simply because of the ease of being manipulated due to the individuals being economically disadvantaged or ill or a racial minority — all three of which apply in this case.
Lack of informed consent
The concept of informed consent, as it applies to medical research, is the basic idea that research subjects have the opportunity to choose whether or not to be part of a research study and that they have sufficient information about what their involvement means (what they will allow to happen to them). The concept was not widely developed and codified at the time of the Tuskegee Syphilis Study. However, both the Nuremberg Code, issued in 1947 to deal with the atrocities of Nazi human experimentation, and the Declaration of Helsinki, issued in 1964 to deal with the ethics of medical research with human subjects, advance the importance of informed consent.
The Nuremberg Code, for example, has as its first principle: "The voluntary consent of the human subject is absolutely essential." A great deal of attention is spent in the Nuremberg Code on explicating what is meant by voluntary consent, including the importance that the subject be provided sufficient knowledge of what the experiment entails.
This means that the person involved should have legal capacity to give consent; should be so situated as to be able to exercise free power of choice, without the intervention of any element of force, fraud, deceit, duress, over-reaching or other ulterior form of constraint or coercion; and should have sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision. The latter element requires that before the acceptance of an affirmative decision by the experimental subject there should be made known to him the nature, duration, and purpose of the experiment; the method and means by which it is to be conducted; all inconveniences and hazards reasonably to be expected; and the effects upon his health or person which may possibly come from his participation in the experiment.
The Declaration of Helsinki also places an emphasis on informed consent. Indeed, the section on informed consent is the most extensive section of the Declaration of Helsinki, over one-quarter of the statement. The Declaration states, for example: "each potential subject must be adequately informed of the aims, methods, sources of funding, any possible conflicts of interest... anticipated benefits and potential risks...The potential subject must be informed of the right to refuse to participate in the study or to withdraw consent to participate at any time without reprisal."
The Tuskegee Syphilis Study continued beyond the dates of the Nuremberg Code and the Declaration of Helsinki, but informed consent was never part of the Tuskegee Study. The subjects did not have an adequate understanding of of the nature of the research in which participating. They did not understand that the purpose was to document the natural course of their illness (until death and autopsy once the study was extended) and without treatment.
As noted by Thomas and Crouse Quinn, "participants were not informed that they suffered from a specific, definable disease that was contagious and transmitted through sexual intercourse."
Brandt's comment on the issue is especially poignant: "The records in the National Archives make clear that the men did not submit voluntarily to an experiment; they were told and they believed that they were getting free treatment from expert government doctors for a serious disease" (Brandt 1978).
Use of deception
Subjects in the study were given the understanding that they were receiving beneficial medical care, such as treatment for "bad blood," not that this was a study to document their medical deterioration without treatment. Some of the tests were presented as if to help the subjects, such as the spinal taps, but were done simply for the benefit of the researchers. Thomas and Crouse Quinn (1991) note, "Syphilis became 'bad blood,' a phrase that Black people of the rural south used to describe a variety of aliments. Consequently, when the PHS physicians announced that they had come to test for 'bad blood,' people turned out in droves."
The spinal tap to test for neurosyphilis, an exam with the risk of considerable pain and complications, was presented as a "special treatment." The letter to the subjects included the following (Brandt 1978):
Some time ago you were given a thorough examination and since that time we hope you have gotten a great deal of treatment for bad blood. You will now be given your last chance to get a second examination. This examination is a very special one and after it is finished you will be given a special treatment if it is believed you are in a condition to stand it....REMEMBER THIS IS YOUR LAST CHANCE FOR SPECIAL FREE TREATMENT. BE SURE TO MEET THE NURSE.
Dr. O. C. Wenger, chief of a federally operated venereal disease center, warned Dr. Raymond Vonderlehr, who originally worked under Dr. Taliaferro Clark and would succeed him as Chief of the Venereal Disease Division, that it is important the men not realize they would be autopsied. He stated in a letter, "there is one danger in the latter plan and that is if the colored population become aware that accepting free hospital care means a post-mortem, every darkey will leave Macon County." Dr. Raymond Vonderlehr responded, "it is not my intention to let it be generally known that the main object of the present activities is bringing of the men to necropsy."
Brandt (1978) noted: "the men participated in the study under the guise of treatment" and "deceit was integral to the study." He further observed that because the men thought they were under the care of government doctors, they largely saw no need to seek treatment elsewhere.
Withholding of treatment
The Tuskegee Syphilis Study was predicated, from its very formation, on the subjects not getting treatment. If the subjects with syphilis were treated, it would go against the plan of the architects of the study. Thus, even though there were treatments available since the study's inception, efforts were made to deprive the subjects of treatment. These efforts became more indefensible after the discovery of an effective and otherwise widely employed treatment, penicillin.
Brandt (1978) wrote that "implicit was the assumption that no adequate therapy existed prior to penicillin. Nonetheless, medical authorities firmly believed in the efficacy of arsenotherapy for treating syphilis at the time of the experiment's inception in 1932...the entire study had been predicated on nontreatment. Provision of effective medication would have violated the rationale of the of the experiment — to study the natural course of the disease until death." He further noted, "while the USPHS believed the experiment might demonstrate that antisyphilitic treatment was unnecessary," considering cases of latent syphilis where no symptoms occurred, "every major textbook of syphilis at the time of the Tuskegee Study's inception strongly advocated treating syphilis even in its latent stages." Among impacts of the study design were that not only could "untreated syphilis lead to cardiovascular disease, insanity, and premature death," but even patients with latent syphilis have the potential to be infectious for others.
After World War II, penicillin became widely available as an effective treatment for syphilis. However, it was deliberately withheld from the subjects, including coordinating with other agencies and physicians to deprive the men of treatment. Thomas and Crouse Quinn (1991) note:
The ultimate tragedy of the Tuskegee experiment was exemplified by the extraordinary measures taken to ensure that subjects in the experimental group did not receive effective treatment. During World War II, approximately 50 of the syphilitic cases received letters from the local draft board ordering them to take treatment. At the request of the PHS, the draft board agreed to exclude the men in the study from its list of draftees needing treatment....In 1943, the PHS began to administer penicillin to syphilitic patients in selected treatment clinics across the nation. The men of the Tuskegee Syphilis Study were excluded from this treatment for the same reason other drugs had been withheld since the beginning of the study in 1932 — treatment would end the study. Once penicillin became the standard of treatment for syphilis in 1951, the PHS insisted that it was all the more urgent for the Tuskegee study to continue because "it made the experiment a never-again-to-be-repeated opportunity."
In the early 1950s, when some were getting treatment, Dr. Vadnderlehr wrote to a participating physician, "I hope that the availability of antibiotics has not interfered too much with this project." It was noted that about thirty percent had secured some treatment, but only about 7.5 percent received what would be considered adequate doses (Brandt 1978).
Brandt (1978) summarizes this ethical failing as follows:
During the forty years of the experiment, the USPHS had sought on several occasions to ensure that the subjects did not receive treatment from other sources. To this end, Vonderlehr met with groups of local Black doctors in 1934 to ask their cooperation in not treating the men. Lists of subjects were distributed to Macon County physicians along with letters requesting them to refer these back to the USPHS if they sought care. The USPHS warned the Alabama Health Department not to treat the test subjects when they took a mobile VD unit into Tuskegee in the early 1940s. In 1941, the Army drafted several subjects and told them to begin antisyphilitic treatment immediately. The USPHS supplied the draft board with a list of 256 names they desired to be excluded from treatment, and the board complied.
Undue influence
Ethical codes for human subject research, such as the Belmont Report, stress that the human subjects be free from the issue of coercion and undue influence, such as improper rewards for participating or individuals in positions where those in authority may place unjustifiable pressure on them. In the case of the Tuskegee Syphilis Study, incentives were offered that provided a strong influence on the decision of subjects to participate and remain in the program, such as free hot lunches, transportation, and medical care for individuals that mostly lacked any access to health care. For individuals in extreme poverty, this offered significant incentives. To get to persuade the men to come to the hospital when severely ill, they were promised that their burial expenses would be covered. Brandt (1978) noted that this last provision "was a particularly strong inducement as funeral rites constituted an important component of the cultural life of rural Blacks."
Racism
Paul and Brookes (2015) state, "the Tuskegee syphilis study in Macon County, Alabama, has been described as an egregious case of blatant racism." Brandt (1978) notes:
The Tuskegee Study reveals the persistence of beliefs within the medical profession about the nature of Blacks, sex, and disease — beliefs that had tragic repercussions long after their alleged "scientific" bases were known to be incorrect....There can be little doubt that the Tuskegee researchers regarded their subjects as less than human....In retrospect, the Tuskegee Study revealed more about the pathology of racism than it did about the pathology of syphilis.
Subsequent Impacts
The Tuskegee Syphilis Study catalyzed a series of events, becoming a milestone in awareness of unethical human subject research and development of regulations to protect such subjects.
The revelations about the Tuskegee Syphilis Study and the subsequent public concern was the main catalyst for conducing a series of congressional subcommittee hearings in February and March of 1973, directed by Senator Edward Kennedy. (There were other unethical research endeavors with human subjects, some also high profile, that contributed as well.)
Largely spurred by the Tuskegee Syphilis Study, the U.S. Congress passed in 1974 the National Research Act, which was signed into law by U.S. President Richard M. Nixon on July 12, 1974. This law was in response to concerns regarding the exploiting and harming of human subjects in medical, biomedical, and social science research. This Act both established the modern system of Institutional Review Boards (IRBs) and created the National Commission for Protection of Human Subjects of Biomedical and Behavior Research. This commission, which had the goal of identifying ethical guidelines for human subject research, would issue a number of reports between 1975 and 1978 dealing with the conduct of research in various populations, such as research involving children, prisoners, pregnant women, and people with dementia. In 1978, the commission issued the Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research; the three main principles identified in this report are widely used to guide human subject research. Amdur and Bankert (2022) note regarding the Tuskegee Syphilis Study: "This study was the main reason that the principle of justice was developed in the Belmont Report."
Following the direction of the National Research Act, the main IRB regulations were established by diverse government agencies. Ultimately, this gave rise to the Common Rule, a federal policy governing the protection of human research subjects as uniformly codified in separate regulations of numerous United States departments and agencies.
On July 23, 1973, a class-action lawsuit seeking $ 1.8 billion was filed in the U.S. District Court for the Middle District of Alabama on behalf of the study participants. There was an out-of-court settlement in December 1974 in which the government agreed to pay $10 million.
On May 16, 1997, the President of the United States, William J. Clinton, issued a formal apology for the role of the United States in the study. He brought some of the survivors and some of the descendants to the White House for this official apology. His statement was unequivocal: "The United States government did something that was wrong — deeply, profoundly, morally wrong. It was an outrage to our commitment to integrity and equality for all our citizens ... and I am sorry.
Another impact of the study is what some have called the "Tuskegee Effect." It is a distrust some segments of the African-American community have regarding medical research and in some cases resulting of under-representation of African-American men in key medical studies (Baker et al. 2005). Thomas and Crouse Quinn (1991) called the Tuskegee Syphilis Study "a historical marker for the legitimate discontent of Blacks with the public health system."
See also
- Belmont Report
- Common Rule
- Declaration of Helsinki
- Human subject research
- Informed consent
- Nuremberg Code
References
ISBN links support NWE through referral fees
- Amdur, Robert J., and Elizabeth A. Bankert. 2022. Institutional Review Book: Member Handbook, 4th Edition. Burlington, MA: Jones & Bardett Learning.
- Baker, Shamim M., Otis W. Brawley, and Leonard S. Marks. 2005. Effects of untreated syphilis in the Negro male, 1932 to 1972: A closure comes to the Tuskegee study, 2004. Urology 65(6): 1259-1262.
- Brandt, Allan M. 1978. Racism and research: the case of the Tuskegee Syphilis Study. The Hastings Center Report 8(6): 21-29.
- Clark, Taliaferro. 1932. The Control of Syphilis in Southern Rural Areas (Chicago: Julius Rosenwald Fund). Cited in Allan M. Brandt, 1978, Racism and research: the case of the Tuskegee Syphilis Study. The Hastings Center Report 8(6): 21-29.
- Heller, Jean. 1972. Syphilis victims in U.S. study went untreated for 40 years. New York Times July 26, 1972.
- McVean, Ada. 2019. 40 years of human experimentation in America: The Tuskegee Study. Office for Science and Society (OSS) Newsletter January 25, 2019.
- New York Times. 1972. Aide questioned syphilis study. New York Times August 9, 1972.
- Paul, Charlotte, and Barbara Brookes. 2015. The rationalization of unethical research: revisionist accounts of the Tuskegee Syphilis Study and the New Zealand "Unfortunate Experiment." American Journal of Public Health 105(10): e12-19.
- Thomas, Stephen B., and Sandra Crouse Quinn. 1991. The Tuskegee Syphilis Study, 1932 to 1972: Implications for HIV education and AIDS risk education programs in the Black community. American Journal of Public Health 81(11): 1498-1505.
Credits
This article began as an original work prepared for New World Encyclopedia and is provided to the public according to the terms of the New World Encyclopedia:Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Any changes made to the original text since then create a derivative work which is also CC-by-sa licensed. To cite this article click here for a list of acceptable citing formats.
Note: Some restrictions may apply to use of individual images which are separately licensed.↧ Download as ZWI file | Last modified: 02/04/2023 10:25:01 | 20 views
☰ Source: https://www.newworldencyclopedia.org/entry/Tuskegee_Syphilis_Study | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed:

 KSF
KSF