Inflammation
 From Nwe
From Nwe
Inflammation is a localized protective response of a body's living tissue to injury, infection, irritation, or allergy. Inflammation is characterized by the following quintet: Redness (rubor), heat (calor), swelling (tumor), pain (dolor), and dysfunction of the organs involved (functio laesa). The first four characteristics have been known since ancient times and are attributed to Roman encyclopedist Celsus (25 B.C.E.—50); functio laesa was added to the definition of inflammation by Rudolf Virchow, in 1858.
Inflammation is part of the innate immune system, that is, the immediate "first-line" of defense to illness or pathogens, which is also known as a nonspecific defense. This is as opposed to the adaptive (acquired) immunity involving antibodies or T-cells that specifically target particular pathogens, but which takes time, usually days, to develop. Inflammation reveals a stunning complexity and harmony to the body, where such actions take place as blood vessels dilating upstream of an infection and constricting downstream, movement of fluid and white blood cells into the area, release of protein and peptide signaling compounds, and so forth.
Inflammation is usually indicated by using the English suffix "-itis," such as appendicitis, laryngitis, pancreatitis, hepatitis, and encephalitis for inflammation of the appendix, larynx, pancreas, liver, and brain, respectively.
Inflammation is not "healthy" nor "unhealthy" on its own. Inflammation helps fight disease or injury, such as by removing pathogens and debris, and walling off infection from spreading. However, it comes at the cost of suspending the body's normal immune and catabolic processes. In the short term, this is often a valid trade-off, but in the long term it causes progressive damage.
Inflammation is not a synonym for infection. Even in cases when it is caused by infection it is incorrect to use the terms as synonyms—Infection is caused by an outside agent, while inflammation is the body's response.
Overview
Inflammation has two main components: Cellular and exudative.
The cellular component involves the movement of white blood cells, or leukocytes, from blood vessels into the inflamed tissue. The white blood cells take on an important role in inflammation; they extravasate (filter out) from the capillaries into tissue, and act as phagocytes, picking up bacteria and cellular debris. They may also aid by walling off an infection and preventing its spread.
Various leukocytes are involved in the initiation and maintenance of inflammation. Generally speaking, acute inflammation is mediated by granulocytes or polymorphonuclear leukocytes, while chronic inflammation is mediated by mononuclear cells, such as monocytes and macrophages. These cells can be further stimulated to maintain inflammation through the action of an adaptive cascade involving lymphocytes: T cells, B cells, and antibodies. These inflammatory cells are:
- Mast cells, which release histamine and prostaglandin in response to activation of stretch receptors. This is especially important in cases of trauma.
- Macrophages, which release TNF-α, IL-1 in response to activation of toll-like receptors.
The exudative component of inflammation involves the movement of fluid, usually containing many important proteins such as fibrin and immunoglobulins (antibodies). (An exudate is any fluid that filters from the circulatory system into lesions or areas of inflammation.) Blood vessels are dilated upstream of an infection (causing redness and heat) and constricted downstream, while capillary permeability to the affected tissue is increased, resulting in a net movement of blood plasma into the tissue, giving rise to edema or swelling. The swelling distends the tissues, compresses nerve endings, and thus causes pain. Inflammation can be recognized by nitric oxide.
If inflammation of the affected site persists, released cytokines IL-1 and TNF will activate endothelial cells to up-regulate receptors VCAM-1, ICAM-1, E-selectin, and L-selectin for various immune cells. (Cytokines are a group of proteins and peptides that are used in organisms as signaling compounds, allowing one cell to communicate with another.) Receptor upregulation increases extravasation of neutrophils, monocytes, activated T-helper, and T-cytotoxic, and memory T, and B cells to the infected site.
Neutrophils are characteristic of inflammation in the early stages. They are the first cells to appear in an infected area, and any section of recently inflamed (within a couple of days or so) tissue viewed under a microscope will appear packed with them. They are easily identified by their multilobed nuclei and granular cytoplasm and perform many important functions, including phagocytosis and the release of extracellular chemical messengers. Neutrophils only live for a couple days in these interstitial areas, so if the inflammation persists for a longer duration then they are gradually replaced by longer lived monocytes.
Outcomes
The outcome in a particular circumstance will be determined by the tissue in which the injury has occurred and the injurious agent that is causing it.
There are four possible results to inflammation:
- Resolution, the complete reconstitution of damaged tissue, does not usually occur in the body.
- Connective tissue scarring. Some 24 hours after inflammation in a wound first occurs, the wound healing response will commence. This response involves the formation of connective tissue to bridge the gap caused by injury and the process of angiogenesis, the formation of new blood vessels, to provide nutrients to the newly formed tissue. Often healing can not occur completely and a scar will form; for example after laceration to the skin, a connective tissue scar results which does not contain any specialized structures such as hair or sweat glands.
- Abscess formation is found primarily in infections by bacteria.
- Ongoing or chronic inflammation. If the injurious agent continues, chronic inflammation will ensue. This process, marked by inflammation lasting many days, months, or even years, may lead to the formation of a chronic wound. Chronic inflammation is characterized by a dominating presence of macrophages in the injured tissue, which extravasate via the same methods discussed above (ICAM-1 VCAM-1). These cells are powerful defensive agents of the body, but the toxins they release (including reactive oxygen species) are injurious to the organism's own tissues as well as invading agents. This is why chronic inflammation is almost always accompanied by tissue destruction. Finally, an abscess, or a collection of pus, can form in chronic inflammation.
Systemic inflammation
Sepsis
When inflammation overwhelms the whole organism, systemic inflammatory response syndrome (SIRS) is diagnosed. When it is due to infection, the term sepsis is applied. Vasodilation (where blood vessels in the body become wider, reducing blood pressure) and organ dysfunction are serious problems that may lead to septic shock and death.
Low-grade
With the discovery of interleukins (group of cytokines, secreted signaling molecules), another concept of systemic inflammation developed. Although the processes involved are identical, this form of inflammation is not confined to a particular tissue but involves the endothelium (lining of blood vessels) and many other organ systems. High levels of several inflammation-related markers such as IL-6, IL-8, and TNF-α are associated with obesity (Bastard et al. 2000, Mohamed-Ali 2001). These levels are reduced in association with increased levels of anti-inflammatory molecules within four weeks after patients begin a very low calorie diet (Clement 2004). The role of systemic inflammation as a cause and/or result of insulin resistance and atherosclerosis is the subject of intense research. It has little direct bearing on clinical care.
Inflammation examples
Inflammation is usually indicated by adding the suffix "-itis," as shown below. However, some conditions such as asthma and pneumonia do not follow this convention.
- Appendicitis (or epityphlitis) is a condition characterized by inflammation of the appendix. While mild cases may resolve without treatment, most require removal of the inflamed appendix, either by laparotomy or laparoscopy. Untreated, mortality is high, mainly due to peritonitis and shock.
- Gastritis is inflammation of the gastric mucosa. The word comes from the Greek gastro- meaning of the stomach and -itis meaning inflammation. Depending on the cause, it may persist acutely or chronically. Most cases are due to Helicobacter pylori bacterial infection.
- Laryngitis is an inflammation of the larynx. It causes hoarse voice or the complete loss of the voice because of irritation to the vocal folds (vocal cords).
- Meningitis is inflammation of the meninges (the membranes covering the central nervous system).
- Otitis is inflammation of the ear.
- Pancreatitis is inflammation of the pancreas.
- Dermatitis is inflammation of the skin (commonly referred to as Eczema)
References
ISBN links support NWE through referral fees
- Bastard, J.-P., C. Jardel, E. Bruckert, P. Blondy, J. Capeau, M. Laville, H. Vidal, and B. Hainque. 2000. Elevated levels of interleukin 6 are reduced in serum and subcutaneous adipose tissue of obese Women after weight loss." The Journal of Clinical Endocrinology & Metabolism 85(9): 3338-3342.
- Clement, K., N. Viguerie, C. Poitou, C. Carette, V. Pelloux, et al. 2004. Weight loss regulates inflammation-related genes in white adipose tissue of obese subjects. FASEB Journal 18:1657-1669. Retreived March 18, 2007.
- Mohamed-Ali, V., L. Flower, J. Sethi, G. Hotamisligil, R. Gray, S. E. Humphries, D. A. York, and J. Pinkney. 2001. ß-Adrenergic Regulation of IL-6 Release from Adipose tissue: In vivo and in vitro studies. The Journal of Clinical Endocrinology & Metabolism 86(12): 5864-5869. Retrieved March 18, 2007.
| Immune system - edit |
|---|
| Humoral immune system | Cellular immune system | Lymphatic system | White blood cells | Antibodies | Antigen (MHC) | Complement system | Inflammation | Clotting factors |
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
↧ Download as ZWI file | Last modified: 02/04/2023 08:14:58 | 88 views
☰ Source: https://www.newworldencyclopedia.org/entry/Inflammatory | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed: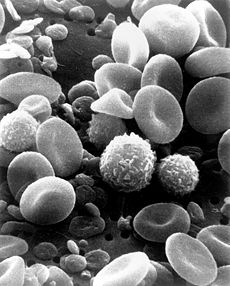
 KSF
KSF