Nursing
 From Nwe
From Nwe -
"Nurse" redirects here.
| Nurse | |
 A British nurse caring for a baby |
|
| Occupation | |
|---|---|
| Names | Nurse |
| Activity sectors | Nursing |
| Description | |
| Competencies | Caring for general well-being of patients |
| Education required | Qualifications in terms of statutory regulations according to national, state, or provincial legislation in each country |
| Fields of employment |
|
| Related jobs | |
Nursing is a profession within the health care sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other health care providers by their approach to patient care, training, and scope of practice. Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient's family, and other team members that focuses on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of a multidisciplinary health care team such as therapists, medical practitioners, and dietitians. In some countries, including the United States and the United Kingdom, advanced practice nurses, such as clinical nurse specialists and nurse practitioners, diagnose health problems and prescribe medications and other therapies. Nurses fulfill a vital function in human society, providing health care both interdependently, such as with physicians, and independently as nursing professionals.
Definition
Although nursing practice varies both through its various specialties and countries, these nursing organizations offer the following definitions:
Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. (International Council of Nurses)[1]
The use of clinical judgment in the provision of care to enable people to improve, maintain, or recover health, to cope with health problems, and to achieve the best possible quality of life, whatever their disease or disability, until death. (Royal College of Nursing)[2]
Nursing is the protection, promotion, and optimization of health and abilities; prevention of illness and injury; alleviation of suffering through the diagnosis and treatment of human responses; and advocacy in health care for individuals, families, communities, and populations. (American Nurses Association)[3]
The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that he would perform unaided if he had the necessary strength, will or knowledge. (Virginia Avenel Henderson)[4]
History
Nursing historians face the challenge of determining whether care provided to the sick or injured in antiquity was nursing care.[5] In the fifth century B.C.E., for example, Hippocrates describes the giving of skilled care and observation of patients by "attendants," who could be considered as early nurses.[6]
Before the foundation of modern nursing, members of religious orders such as nuns and monks often provided nursing-like care. These are found, for example, in Christian,[7] Islamic[8] and Buddhist[9] traditions. These traditions were influential in the development of the ethos of modern nursing.
During the Reformation of the sixteenth century, Protestant reformers shut down the monasteries and convents, allowing a few hundred municipal hospices to remain in operation in northern Europe. Nursing care went to the inexperienced as traditional caretakers, rooted in the Roman Catholic Church, were removed from their positions. As a result, the nursing profession suffered a major setback for approximately 200 years.[10]
Nineteenth century
During the Crimean War the Grand Duchess Elena Pavlovna issued the call for women to join the Order of Exaltation of the Cross (Krestodvizhenskaya obshchina) for the year of service in the military hospitals. The first section of twenty-eight "sisters," headed by Aleksandra Petrovna Stakhovich, the Directress of the Order, went off to the Crimea early in November 1854.[11]

Florence Nightingale laid the foundations of professional nursing after the Crimean War.[12] From 1870, having set up the first school of nursing connected to a continuously operating hospital and medical school, the Nightingale model of professional education spread widely in Europe and North America.[13] Often considered the first nurse theorist, Nightingale linked health with five environmental factors:(1) pure or fresh air, (2) pure water, (3) efficient drainage, (4) cleanliness, and (5) light, especially direct sun light. Deficiencies in these five factors resulted in lack of health or illness.[14] Nightingale was also a pioneer of the graphical presentation of statistical data.[15]
The following were also important in the development of the nursing profession in the nineteenth century:
- Agnes Jones, of Fahan, County Donegal, Ireland became the first trained Nursing Superintendent of Liverpool Workhouse Infirmary at Brownlow Hill in 1865, and established a nurse training regime there.[16]
- Linda Richards, who was the first professionally trained nurse in the US graduated in 1873 from the New England Hospital for Women and Children in Boston, established quality nursing schools in the United States and Japan. She served as the first president of the American Society of Superintendents of Training Schools in 1894, which was the first professional organization for nurses.[17]
- Clarissa Harlowe "Clara" Barton, a pioneer American teacher, patent clerk, nurse, and humanitarian, and the founder of the American Red Cross.[18]
- Saint Marianne Cope, a Sister of St. Francis who opened and operated some of the first general hospitals in the United States, instituting cleanliness standards which influenced the development of America's modern hospital system.[19]
- Agnes Hunt from Shropshire was the first orthopedic nurse and was pivotal in the emergence of the The Robert Jones and Agnes Hunt Orthopaedic Hospital in Oswestry, Shropshire, UK.[20]
Catholic orders such as Little Sisters of the Poor, Sisters of Mercy, Sisters of St. Mary, St. Francis Health Services, Inc., and Sisters of Charity built hospitals and provided nursing services during this period.
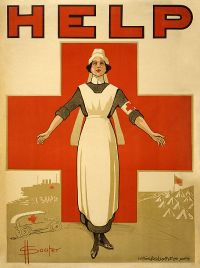
Twentieth century
Hospital-based training came to the fore in the early 1900s, with an emphasis on practical experience. The Nightingale-style school began to disappear.
Many nurses saw active duty in World War I, but the profession was transformed during the Second World War. British nurses of the Army Nursing Service were part of every overseas campaign.[21] More nurses volunteered for service in the US Army and Navy than any other occupation.[22] The Nazis had their own Brown Nurses, 40,000 strong.[23] Two dozen German Red Cross nurses were awarded the Iron Cross for heroism under fire.[24]
Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles have been changing.[25]
The modern era saw the development of undergraduate and post-graduate nursing degrees. Advancement of nursing research and a desire for association and organization led to the formation of a wide variety of professional organizations and academic journals in the field. Growing recognition of nursing as a distinct academic discipline was accompanied by an awareness of the need to define the theoretical basis for practice.[26]
In the nineteenth and early twentieth century, nursing was considered a women's profession, just as doctoring was a men's profession. With increasing expectations of workplace equality during the late twentieth century, nursing became an officially gender-neutral profession. In practice, however, the percentage of male nurses remained well below that of female physicians in the early twenty-first century.
As a profession
Nurses care for individuals of all ages and cultural backgrounds who are healthy and ill in a holistic manner based on the individual's physical, emotional, psychological, intellectual, social, and spiritual needs. The profession combines physical science, social science, nursing theory, and technology in caring for those individuals. The authority for the practice of nursing is based upon a social contract that delineates professional rights and responsibilities as well as mechanisms for public accountability. In almost all countries, nursing practice is defined and governed by law, and entrance to the profession is regulated at the national or state level.
The aim of the nursing community worldwide is for its professionals to ensure quality care for all, while maintaining their credentials, code of ethics, standards, and competencies, and continuing their education. There are a number of educational paths to becoming a professional nurse, which vary greatly worldwide; all involve extensive study of nursing theory and practice as well as training in clinical skills.
To work in the nursing profession, all nurses hold one or more credentials depending on their scope of practice and education. In the United States, a Licensed Practical Nurse (LPN) will work under the direction of a physician, mid-level practitioner, or Registered Nurse (RN). RNs provide scientific, psychological, and technological knowledge in the care of patients and families in many health care settings.
In the United States, multiple educational paths will qualify a candidate to sit for the licensing examination as an RN. The Associate Degree in Nursing (ADN) is awarded to the nurse who has completed a two-year undergraduate academic degree awarded by community colleges, junior colleges, technical colleges, and bachelor's degree-granting colleges and universities upon completion of a course of study usually lasting two years. The Bachelor of Science in Nursing (BSN) is awarded to the nurse who has earned an American four-year academic degree in the science and principles of nursing, granted by a tertiary education university or similarly accredited school. After completing either the LPN or either RN education programs in the United States, graduates are eligible to sit for a licensing examination to become a nurse, the passing of which is required for the nursing license.[27]
Scope of activities
RNs treat patients, record their medical history, provide emotional support, and provide follow-up care. Nurses also help doctors perform diagnostic tests, and may also assist doctors in the emergency room or in trauma care when help is needed.[28]
Activities of daily living assistance
Assisting in activities of daily living (ADL) are skills required in nursing as well as other professions such as nursing assistants. This includes assisting in patient mobility, such as moving an activity intolerant patient within bed. For hygiene, this often involves bed baths and assisting with urinary and bowel elimination.
Medication
All medications administered by nurses must be from a medication prescription from a licensed practitioner, such as a physician. Nurses do not have the authority to prescribe medications, although there are some exceptions. Nurses are legally responsible for the drugs they administer. There may be legal implications when there is an error in a prescription, and the nurse could be expected to have noted and reported the error. In the United States, nurses have the right to refuse any medication administration that they deem to be potentially harmful to the patient.[29]
In the United States, credentialed nurse practitioners (NP) can prescribe medication, including controlled substances. However, their degree of independence varies by state: In several states nurse practitioners have the explicit legal authority to prescribe; in others they must have a “collaborative relationship” or “protocol agreement” with a specific, supervising physician in order to prescribe medication.[30] A number of other countries around the world, including 13 European nations, allow qualified nurses to prescribe medication, some with full prescribing rights and others have restricted prescribing rights.[31]
Patient education
Patient education is the process by which health professionals and others impart information to patients and their caregivers that will alter their health behaviors or improve their health status. The patient's family is often involved in the education. Effective patient education leads to fewer complications and hospital visits.[29]
Specialties
Nursing is a very diverse health care profession. Nurses practice in a wide range of settings; some nurses follow the traditional role of working in a hospital setting while other work in more specialized settings such as private homes, schools, long-term care facilities, pharmaceutical companies, and as researchers in laboratories, universities, and research institutions.
Generally nursing is divided according to the needs of the patients. The major populations are:
- communities/public
- family/individual across the lifespan
- adult-gerontology
- pediatrics
- neonatal
- women's health/gender-related
- mental health
- informatics (eHealth)
- acute care hospitals
- ambulatory settings (physician offices, urgent care settings, camps, etc)
- school/college infirmaries
There are also specialist areas such as cardiac nursing, orthopedic nursing, palliative care, perioperative nursing, obstetrical nursing, oncology nursing, nursing informatics, telenursing, radiology, and emergency nursing.
Occupational hazards
The fast-paced and unpredictable nature of health care places nurses at risk for injuries and illnesses, including high occupational stress. Nurses consistently identify stress as a major work-related concern and have among the highest levels of occupational stress when compared to other professions. This stress is caused by the environment, psychosocial stressors, and the demands of nursing, including new technology that must be mastered, the emotional labor involved in nursing, physical labor, shift work, and high workload. This stress puts nurses at risk for short-term and long-term health problems, including sleep disorders, depression, mortality, psychiatric disorders, stress-related illnesses, and illness in general. Nurses are at risk of developing compassion fatigue and moral distress, which can worsen mental health. They also have very high rates of occupational burnout and emotional exhaustion, which increase the risk for illness, medical error, and suboptimal care provision.[32]
Nurses are also at risk for violence and abuse in the workplace.[33] Violence is typically perpetrated by non-staff (such as patients or family), whereas abuse is typically perpetrated by other hospital personnel.
Prevention
There are a number of interventions that can mitigate the occupational hazards of nursing. Individual-focused interventions include stress management programs, which can be customized to individuals, and which can reduce anxiety, sleep disorders, and other symptoms of stress. Physical supports, such as lumbar supports for the back, may also be used to reduce physical injury and alleviate pain.[34].[35] Organizational interventions focus on reducing stressful aspects of the work environment by defining stressful characteristics and developing solutions to them. Using organizational and individual interventions together is most effective at reducing stress on nurses.[32]
Shortage of nurses
Internationally, there is a serious shortage of nurses.[36] One reason for this shortage is due to the work environment in which nurses practice. In a recent review of the empirical human factors and ergonomic literature specific to nursing performance, nurses were found to work in generally poor environmental conditions. Some countries and states have passed legislation regarding acceptable nurse-to-patient ratios.
Notes
- ↑ Definition of Nursing ICN, 2002. Retrieved April 1, 2020.
- ↑ Helen Scott, RCN's definition of nursing: what makes nursing unique? British Journal of Nursing 11(21) (September 27, 2013). Retrieved April 1, 2020.
- ↑ Scope of practice defined in nursing ANA. Retrieved April 1, 2020.
- ↑ Angelo Gonzalo, Virginia Henderson: Nursing Need Theory Nurseslabs. Retrieved April 1, 2020.
- ↑ Chad E. O'Lynn and Russell E. Tranbarger (eds.), Men in Nursing: History, Challenges, and Opportunities (Springer Publishing Company, 2006, ISBN 978-0826102218).
- ↑ Edwin B. Levine and Myra E. Levine, Hippocrates, father of nursing, too? The American Journal of Nursing 65(12) (December 1965):86-88. Retrieved March 30, 2020.
- ↑ Gary B. Ferngren, Medicine and Health Care in Early Christianity (Johns Hopkins University Press, 2016, ISBN 978-1421420066).
- ↑ Abdulaziz Sachedina, Islamic Biomedical Ethics: Principles and Application (Oxford University Press, 2009, ISBN 978-0195378504).
- ↑ William Theodore de Bary, The Buddhist Tradition: In India, China and Japan (Vintage, 1972, ISBN 978-0394716961).
- ↑ Kathleen Masters, Role Development in Professional Nursing Practice (Jones & Bartlett Learning, 2018, ISBN 978-1284152913).
- ↑ John Shelton Curtiss, Russian Sisters of Mercy in the Crimea, 1854-1855 Slavic Review 25(1) (March 1966): 84-100. Retrieved April 2, 2020.
- ↑ Warren Winkelstein, Jr., Florence Nightingale: Founder of Modern Nursing and Hospital Epidemiology Epidemiology 20(2) (March 2009): 311. Retrieved April 2, 2020.
- ↑ Shawna M. Quinn, Agnes Warner and the Nursing Sisters of the Great War (Goose Lane Editions, 2010, ISBN 978-0864926333).
- ↑ Kathy Blais and Janice S. Hayes, Professional Nursing Practice: Concepts and Perspectives (Pearson, 2015, ISBN 978-0133801316).
- ↑ Mark Bostridge, Florence Nightingale: the Lady with the Lamp| BBC, February 17, 2011. Retrieved April 2, 2020.
- ↑ Steven Horton, Agnes Jones Liverpool Hidden History, February 18, 2018. Retrieved April 2, 2020.
- ↑ Linda A.J. Richards 1841 - 1930 American Association for the History of Nursing. Retrieved April 2, 2020.
- ↑ Founder Clara Barton The American National Red Cross. Retrieved April 2, 2020.
- ↑ Jen Christensen, Mother Marianne becomes an American saint CNN, October 22, 2012. Retrieved April 2, 2020.
- ↑ Hospital History The Robert Jones and Agnes Hunt Orthopaedic Hospital. Retrieved April 2, 2020.
- ↑ QA World War Two Nursing Qaranc. Retrieved April 2, 2020.
- ↑ Philip A. Kalisch and Beatrice J. Kalisch, American Nursing: A History (LWW, 2003, ISBN 978-0781739696).
- ↑ Bronny Rebekah McFarland-Icky, Nurses in Nazi Germany (Princeton University Press, 1999, 978-0691006659).
- ↑ Gordon Williamson, World War II German Women's Auxiliary Services (Osprey Publishing, 2003, ISBN 978-1841764078).
- ↑ Lynne M. Dunphy, Jill E. Winland-Brown, Brian Oscar Porter, and Debera J. Thomas, Primary Care: Art and Science of Advanced Practice Nursing - An Interprofessional Approach (F.A. Davis Company, 2019, ISBN 978-0803667181).
- ↑ Martha Raile Alligood, Nursing Theorists and Their Work (Mosby, 2013, ISBN 978-0323091947).
- ↑ Everything Nurses Need to Know About the NCLEX Licensing Exam. Retrieved April 2, 2020.
- ↑ Registered Nurse (RN) Career Profiles. Retrieved April 2, 2020.
- ↑ 29.0 29.1 Carol Taylor, Pamela Lynn, and Jennifer Bartlett, Fundamentals of Nursing: The Art and Science of Person-Centered Care (LWW, 2018, ISBN 978-1496362179).
- ↑ Can Nurse Practitioners Prescribe Medication? 'Nurse Practitioner Schools. Retrieved April 2, 2020.
- ↑ Claudia B. Maier, Nurse prescribing of medicines in 13 European countries Human Resources for Health 17 (2019). Retrieved April 2, 2020.
- ↑ 32.0 32.1 Rashaun Roberts, Paula L. Grubb, and James W. Grosch, Alleviating Job Stress in Nurses Medscape, June 25, 2012. Retrieved April 2, 2020.
- ↑ Dan Hartley and Marilyn Ridenour, Free On-line Violence Prevention Training for Nurses National Institute for Occupational Safety and Health, August 12, 2013. Retrieved April 2, 2020.
- ↑ Anna P. Dawson, Skye N. McLennan, Stefan D. Schiller, Gwendolen A. Jull, Paul W. Hodges, and Simon Stewart, Interventions to prevent back pain and back injury in nurses: a systematic review Occupational and Environmental Medicine, 64(10) (2007): 642–650. Retrieved April 2, 2020.
- ↑ Anna P. Dawson, Skye N. McLennan, Stefan D. Schiller, Gwendolen A. Jull, Paul W. Hodges, and Simon Stewart, Interventions to prevent back pain and back injury in nurses: a systematic review Occupational and Environmental Medicine, 64(10) (2007): 642–650. Retrieved April 2, 2020.
- ↑ James Buchan, Global nursing shortages BMJ 324(7340) (2002): 751–752. Retrieved April 2, 2020.
References
ISBN links support NWE through referral fees
- Alligood, Martha Raile. Nursing Theorists and Their Work. Mosby, 2013. ISBN 978-0323091947
- Blais, Kathy, and Janice S. Hayes. Professional Nursing Practice: Concepts and Perspectives. Pearson, 2015. ISBN 978-0133801316
- D'Antonio, Patricia. American Nursing: A History of Knowledge, Authority, and the Meaning of Work. Johns Hopkins University Press, 2010. ISBN 978-0801895654
- de Bary, William Theodore. The Buddhist Tradition: In India, China and Japan. Vintage, 1972. ISBN 978-0394716961
- Dunphy, Lynne M., Jill E. Winland-Brown, Brian Oscar Porter, and Debera J. Thomas. Primary Care: Art and Science of Advanced Practice Nursing - An Interprofessional Approach. F.A. Davis Company, 2019. ISBN 978-0803667181
- Ferngren, Gary B. Medicine and Health Care in Early Christianity. Johns Hopkins University Press, 2016. ISBN 978-1421420066
- Henderson, Virginia. The Nature of Nursing. National League for Nursing Press, 1991. ISBN 978-0887374944
- Kalisch, Philip A., and Beatrice J. Kalisch. American Nursing: A History. LWW, 2003. ISBN 978-0781739696
- McFarland-Icky, Bronny Rebekah. Nurses in Nazi Germany. Princeton University Press, 1999. 978-0691006659
- Masters, Kathleen. Role Development in Professional Nursing Practice. Jones & Bartlett Learning, 2018. ISBN 978-1284152913
- Nightingale, Florence. Notes on Nursing: What It Is, and What It Is Not. IndoEuropeanPublishing, 2019. ISBN 978-1644390887
- O'Lynn, Chad E., and Russell E. Tranbarger (eds.). Men in Nursing: History, Challenges, and Opportunities. Springer Publishing Company, 2006. ISBN 978-0826102218
- Quinn, Shawna M. Agnes Warner and the Nursing Sisters of the Great War. Goose Lane Editions, 2010. ISBN 978-0864926333
- Roux, Gayle. Issues and Trends in Nursing: Essential Knowledge for Today and Tomorrow. Jones & Bartlett Learning, 2008. ISBN 978-0763752255
- Sachedina, Abdulaziz. Islamic Biomedical Ethics: Principles and Application . Oxford University Press, 2009. ISBN 978-0195378504
- Williamson, Gordon. World War II German Women's Auxiliary Services. Osprey Publishing, 2003. ISBN 978-1841764078
External links
All links retrieved November 16, 2022.
- Royal College of Nursing (RCN)
- International Council of Nurses (ICN)
- American Nurses Association (ANA)
- Nursing Careers & Specialties for RNs
|
|||||||||||||||||
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
↧ Download as ZWI file | Last modified: 02/04/2023 03:30:54 | 106 views
☰ Source: https://www.newworldencyclopedia.org/entry/Nursing | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed:

 KSF
KSF